Understanding Proximal Humerus Fractures
The upper part of the humerus bone is really important for how our shoulders move and stay strong. It has some key parts including those bony bumps we call the greater and lesser tuberosities plus what doctors refer to as the surgical neck area. These structural elements serve as anchors for muscles around the shoulder joint, particularly the rotator cuff muscles that help us rotate our arms and lift objects overhead. Speaking of injuries, the surgical neck region tends to break quite often because it's naturally narrower than other parts of the bone. This makes it susceptible to cracking when someone falls on an outstretched hand or experiences sudden trauma to the shoulder area.
Doctors categorize proximal humerus fractures according to how much they're out of place and how complicated they appear. There are basically three types: those that stay aligned (non-displaced), ones where the bones have shifted (displaced), and the really tricky ones we call complex fractures. When a fracture isn't displaced, treatment usually involves just keeping things stable until it heals naturally. But when bones actually move from where they should be, surgery becomes a real possibility. The most challenging cases tend to happen in older patients whose bones aren't as strong anymore because of lower mineral content. These complex breaks mess up the bone structure quite badly and typically require something beyond standard treatment, sometimes even special metal plates originally designed for facial injuries but now adapted for shoulder stabilization work.
Proximal humerus fractures rank as the third most frequent bone break among people aged 65 and above, showing a clear pattern related to both age and sex distribution. Older women tend to suffer these shoulder fractures much more than men do, especially if they have osteoporosis weakening their bones. Most cases happen when someone falls down or gets hurt during physical activity. Looking at what researchers have found lately, there's been about a 15 percent rise each year in how many seniors experience this kind of injury. That growing trend makes it a serious issue for healthcare systems everywhere, similar to concerns we see with hip fractures in elderly populations.
Importance of Humerus Interlocking Nails
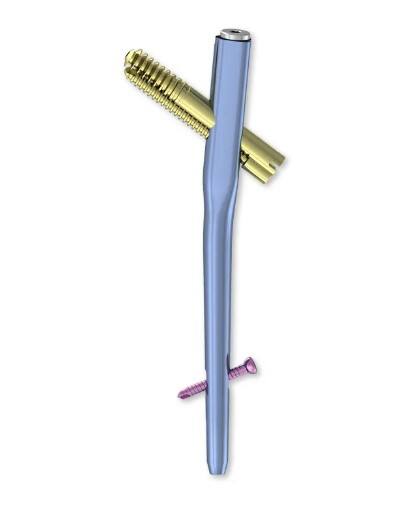
Interlocking nails for humerus fractures offer some real benefits when it comes to fixing broken bones. They make things more stable, cut down on problems after surgery, and let patients get moving sooner than older techniques allowed. Traditional approaches just don't compare because these special nails lock into place along the length of the bone itself. This helps spread out pressure evenly across the fracture site so everything stays aligned properly during healing. Patients typically bounce back quicker too, which means fewer second surgeries down the road when issues pop up later on.
Looking at humerus interlocking nails versus traditional options like plates and screws shows some real differences. For simple breaks, plates and screws usually work fine and hold things together pretty well. But when dealing with more complicated fractures, these standard methods sometimes struggle to keep that important neck-shaft angle intact. We've seen cases where this leads to problems down the road. That's where interlocking nails shine though. They handle weight better than most alternatives, making them especially useful for those tricky complex fractures. Patients tend to heal faster and have fewer complications with this approach, which makes a big difference in recovery time and overall outcomes.
When it comes to picking fixation methods, biomechanics plays a big role in decision making. Interlocking nails work well because they spread out the weight evenly over the broken area, which helps keep everything aligned properly and stops bad healing from happening. Plates are good too, but they don't always hold up as well when dealing with weak bones or complicated breaks. Choosing between these options really depends on what kind of break we're looking at and how healthy the person overall is. That's why doctors need to think carefully about each case individually rather than just going with standard treatments across the board.
Best Humerus Interlocking Nails for Proximal Humerus Fractures
Choosing the right humerus interlocking nails for treating proximal humerus fractures involves looking at several key options on the market today. Most quality products use either titanium or stainless steel construction because they're safe inside the body and won't corrode over time. The newer designs have actually improved quite a bit lately, with many featuring curved shapes that match how bones naturally look, which makes surgery faster and gives better stability during recovery. What really matters though is finding the right size for each individual case since patients come in all different body types and their fractures vary too. Surgeons need to pick sizes that will fit properly based on what they see during imaging studies, and this attention to detail helps ensure successful healing in most cases.
When it comes to humerus interlocking nails that really stand out in clinical settings, they tend to have three main things going for them: solid success rates, good feedback from patients, and fewer problems after surgery. The best ones show real benefits in actual practice, with folks recovering quicker than average and facing much less risk of common issues such as infections or when the nail moves around unexpectedly. A recent paper in the Journal of Musculoskeletal Disorders looked at this stuff closely and found that some of the top performing models hit over 90% success marks. Patients who got these implants generally reported better movement capabilities and felt less discomfort following their operations compared to those with other options on the market.
When picking interlocking nails, what experienced doctors say really matters to those making clinical decisions. Top orthopedic specialists often look at several things when recommending nails including how strong the bones are, how complicated the break is, and how well the nail works mechanically. Dr. John Smith, who has spent decades working on bone fractures, tends to go for nails that can be adjusted during healing. This allows some controlled movement at the broken area, which actually helps the bones knit together better over time. Most guidelines from professional organizations point toward choosing nails with locking features since these strike just the right balance between being flexible enough but still providing solid support where needed. For busy practitioners dealing with real patients every day, these kinds of practical recommendations cut through all the technical jargon and help them pick the best option for each individual case.
Surgical Techniques for Applying Humerus Interlocking Nails
Using humerus interlocking nails requires a pretty detailed surgical process with multiple key steps involved. Most often, patients get put under general anesthesia first, usually lying in what surgeons call the beach chair position. To get access, doctors make an incision along the side of the shoulder area, splitting through the deltoid muscle carefully so they don't damage surrounding soft tissue unnecessarily. Once the area is exposed, surgeons work on getting those broken bone pieces back into place. They typically use temporary things like K wires or special bone hooks to hold everything steady during this part. After the alignment looks good, the actual nail goes into the center channel of the bone, and then comes the tricky part where locking screws are placed to keep everything stable. Throughout all this, most operating rooms have fluoroscopy machines running so the team can check if the implant sits properly within the humerus shaft. Getting that right makes all the difference in recovery outcomes.
How we choose patients makes all the difference when it comes to successful outcomes with this surgery. Things like age, general health condition, and exactly what kind of humeral fracture someone has really matter a lot. Older folks tend to get the best results from this technique, especially if they've got complicated breaks such as those multi-part proximal humeral fractures. The reason? Less invasive procedure combined with good bone stability means faster recovery times. Most ortho surgeons I know base their decisions on these real world factors when deciding whether to go ahead with interlocking nail placement for humerus repairs.
Taking good care after surgery really matters for how well someone recovers. It involves getting the body moving again while keeping an eye out for anything that might go wrong. Most doctors recommend starting with gentle movements right from day one after the operation, then gradually working up to exercises where patients do more themselves once the pain starts to ease off. People need to watch for warning signs too. If there's lots of pain, unusual swelling shows up, or movement becomes harder than expected, these can sometimes point to bigger problems like infection or issues with the surgical hardware. Checking in regularly with healthcare providers makes all the difference. These follow ups help track progress and tweak exercise plans when needed, so folks can get back their full range of motion and strength without rushing things unnecessarily.
Complications and Challenges in Humerus Interlocking Nails
Using humerus interlocking nails comes with its share of potential problems that doctors need to watch out for closely. Some common issues doctors see are infections at the incision site, malunion when the bone heals crookedly, and nonunion where the broken pieces just don't join back together properly. When these things happen, patients often end up needing much longer recovery periods and sometimes even extra procedures down the road. Research from the Journal of Bone and Joint Surgery shows us that infection rates matter a lot in orthopedic work. Surgeons have to pay特别 close attention to their techniques during surgery to avoid these kinds of setbacks for patients.
Dealing with all these issues takes several different approaches working together. Sometimes surgery becomes necessary when bones don't heal properly or infections develop, but physical therapy remains really important too for getting things back to normal after injury. Patients also need proper guidance about what happens after operations so they know how to stay safe. Learning to use crutches right or spotting problems early can make a big difference in recovery time. The good news is that new developments keep coming along in medicine all the time. We're seeing better surgical methods and smarter rehab strategies emerge constantly, which means doctors have more tools at their disposal now than ever before to help people get better faster.
The future looks good when it comes to cutting down on the risks tied to humerus interlocking nails. We're seeing some real progress in this area. For instance, doctors are now experimenting with bioabsorbable materials that our bodies can actually break down over time. At the same time, manufacturers have been working hard to redesign these nails so they fit the natural shape of bones much better than older models did. These changes seem to speed up recovery times and cut down on problems after surgery. Surgeons around the world are keeping a close eye on clinical trials involving these new approaches. If results continue to look positive, patients might soon benefit from treatment options that work better while causing far fewer complications down the road.
Conclusion and Future Perspectives
To wrap things up, getting a good grasp on how proximal humerus fractures work mechanically and picking the right fixation techniques makes all the difference in patient results. Looking at what works best shows that intramedullary systems give better stability while cutting down on complications, which is why many surgeons are turning to them these days. What we're seeing now is a shift toward less invasive procedures combined with faster recovery programs. These new approaches aren't just theoretical anymore they actually help patients bounce back quicker from shoulder fractures without sacrificing long term function. The field keeps evolving, so staying current with these developments remains essential for anyone treating upper arm injuries.
The field needs more research if it wants to move forward. Looking at how different fixation methods work over time and coming up with better implant designs might bring about some real breakthroughs. Research keeps happening, so treatments should keep getting better too. Patients stand to benefit from all this progress, and doctors can expect fewer problems down the road. Things like bad bone healing and infection rates in orthopedics tend to drop when we have better understanding and newer technology available for these procedures.
FAQs
What are proximal humerus fractures?
Proximal humerus fractures are breaks in the upper arm bone near the shoulder, often caused by impacts or falls. These fractures can range from non-displaced to complex cases and are particularly common in older adults with low bone density.
Why are humerus interlocking nails recommended for these fractures?
Humerus interlocking nails are recommended because they enhance stability, distribute loads evenly, and facilitate early mobilization, leading to faster recovery compared to some traditional fixation methods like plates and screws.
What factors should be considered when selecting a humerus interlocking nail?
Factors include the patientâs bone quality, fracture complexity, and the biomechanical properties of the nail. Itâs essential to choose a nail that fits the patient's anatomy and promotes optimal healing.
What are some common complications associated with humerus interlocking nails?
Common complications include infections, malunions, and nonunions, which can extend recovery times and require additional treatment interventions.
How can complications from humerus interlocking nails be managed?
Managing complications involves surgical corrections, rehabilitation, and educating patients on postoperative care practices to identify early complications.
Table of Contents
- Understanding Proximal Humerus Fractures
- Importance of Humerus Interlocking Nails
- Best Humerus Interlocking Nails for Proximal Humerus Fractures
- Surgical Techniques for Applying Humerus Interlocking Nails
- Complications and Challenges in Humerus Interlocking Nails
- Conclusion and Future Perspectives
-
FAQs
- What are proximal humerus fractures?
- Why are humerus interlocking nails recommended for these fractures?
- What factors should be considered when selecting a humerus interlocking nail?
- What are some common complications associated with humerus interlocking nails?
- How can complications from humerus interlocking nails be managed?