Modern spinal surgery has undergone a revolutionary transformation with the advent of minimally invasive surgical techniques, fundamentally changing how spine screws are utilized in patient treatment. These precision-engineered implants have become the cornerstone of contemporary spinal fusion procedures, enabling surgeons to address complex spinal conditions through smaller incisions while maintaining exceptional biomechanical stability. The integration of advanced spine screws in minimally invasive approaches has significantly reduced patient recovery times, minimized tissue trauma, and improved overall surgical outcomes across diverse pathological conditions.
The evolution of spinal instrumentation technology has positioned these specialized implants as essential components in treating degenerative disc disease, spinal stenosis, spondylolisthesis, and traumatic spinal injuries. Through sophisticated design engineering and material science advancements, modern implants deliver superior holding power while facilitating the precise navigation required for minimally invasive surgical corridors. This technological advancement has enabled spine surgeons to achieve optimal fusion outcomes while preserving surrounding anatomical structures and maintaining the integrity of the paraspinal musculature.
Fundamental Principles of Minimally Invasive Spinal Surgery
Surgical Approach Methodology
Minimally invasive spinal surgery represents a paradigm shift from traditional open procedures, utilizing specialized retractor systems and tubular approaches to access the surgical site through muscle-splitting techniques rather than extensive muscle stripping. This methodology preserves the natural muscle attachments to the spinous processes and laminae, significantly reducing postoperative pain and accelerating patient rehabilitation. The surgical corridors created through these techniques provide adequate visualization and working space for precise implant placement while minimizing disruption to surrounding tissues.
The technical execution of minimally invasive procedures requires specialized instrumentation designed specifically for working within confined surgical spaces. Advanced imaging guidance systems, including fluoroscopy and navigation technology, enable surgeons to achieve accurate implant positioning despite limited direct visualization. These technological integrations have made complex spinal reconstructions feasible through minimal access points, fundamentally altering the risk-benefit profile of spinal surgery for patients across all demographic categories.
Anatomical Preservation Strategies
The preservation of anatomical structures during minimally invasive procedures extends beyond muscle tissue to include the preservation of ligamentous structures, facet joint integrity, and segmental blood supply. This comprehensive approach to tissue preservation contributes significantly to improved biomechanical outcomes and reduced adjacent segment degeneration rates. The strategic placement of spine screws through these preserved anatomical corridors maintains the natural load-sharing mechanisms of the spinal column while providing the necessary stability for fusion.
Contemporary surgical techniques emphasize the importance of maintaining the posterior tension band complex, including the supraspinous and interspinous ligaments, whenever possible. This preservation strategy has demonstrated significant benefits in maintaining sagittal balance and reducing the incidence of post-surgical complications. The integration of advanced implant designs with these anatomical preservation principles has resulted in improved long-term clinical outcomes and enhanced patient satisfaction scores across multiple outcome measures.
Biomechanical Engineering of Modern Spinal Implants
Material Science Innovations
The development of contemporary spinal implants incorporates cutting-edge materials science, utilizing titanium alloys and specialized surface treatments to optimize osseointegration while maintaining appropriate mechanical properties. These materials provide the necessary strength-to-weight ratio required for long-term spinal stability while promoting biological integration with the surrounding bone tissue. The surface topography of modern implants includes advanced coatings and texturing that enhance bone ingrowth and reduce the risk of implant loosening over time.
Biocompatibility considerations have driven the selection of materials that minimize inflammatory responses while promoting favorable bone remodeling patterns around the implant interface. The modulus of elasticity of these materials has been carefully engineered to approximate that of human bone, reducing stress shielding effects and promoting more physiologic load transfer through the spinal segments. These material properties contribute significantly to the long-term success rates observed with contemporary spinal fusion procedures.
Design Optimization Features
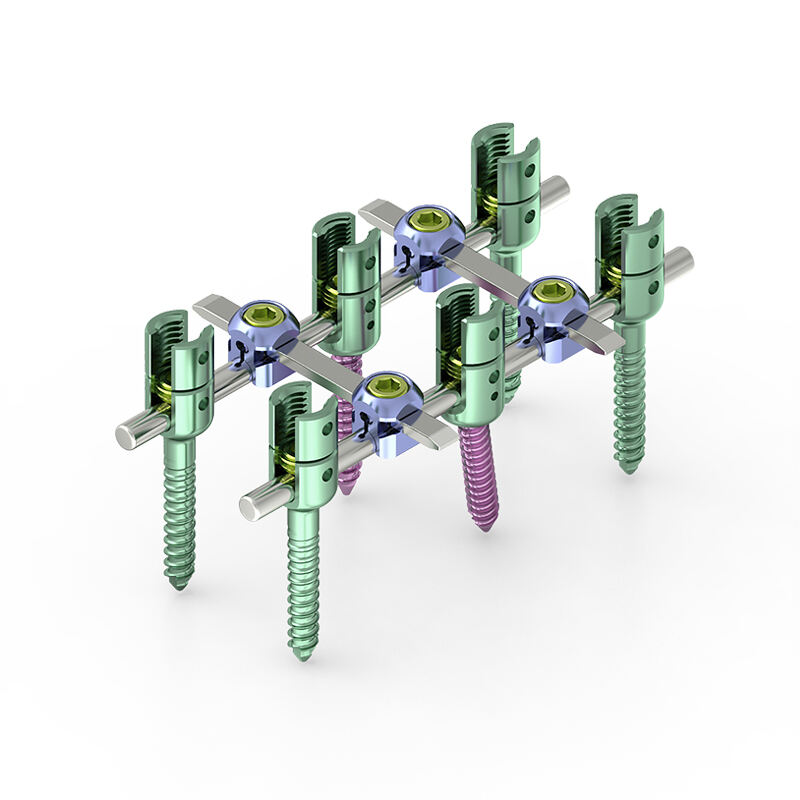
Modern spinal implant design incorporates sophisticated geometric features that optimize both insertion characteristics and long-term fixation strength. The thread design, tip geometry, and core diameter have been extensively analyzed through finite element modeling and biomechanical testing to maximize purchase in both cancellous and cortical bone. These design optimizations enable reliable fixation across varying bone quality conditions, from osteoporotic elderly patients to high-density bone in younger demographics.
The incorporation of self-tapping and self-drilling features has streamlined surgical procedures while reducing the risk of bone damage during implant insertion. These design elements facilitate precise placement through minimally invasive surgical corridors while maintaining optimal trajectory control. The polyaxial head designs common in contemporary systems provide the flexibility necessary for rod placement through limited surgical exposures, enabling complex multi-level constructs through minimal access points.
Surgical Technique Considerations
Trajectory Planning and Navigation
Precise trajectory planning represents a critical component of successful minimally invasive spinal surgery, requiring detailed preoperative analysis of patient anatomy and careful consideration of optimal entry points and screw paths. Advanced imaging modalities, including high-resolution CT scanning and MRI, provide the anatomical detail necessary for surgical planning while identifying potential anatomical variants that could impact surgical approach. The integration of computer-assisted navigation systems has further enhanced trajectory accuracy, reducing the risk of neural or vascular injury during implant placement.
Intraoperative imaging guidance through fluoroscopy or navigation technology enables real-time verification of implant positioning, ensuring optimal placement within the targeted anatomical structures. The use of these guidance systems has significantly reduced the learning curve associated with minimally invasive techniques while improving overall surgical outcomes. The ability to confirm accurate placement before final tightening of the construct provides surgeons with confidence in the biomechanical integrity of the final instrumentation.
Construct Design Principles
The design of spinal constructs for minimally invasive procedures must balance the competing requirements of adequate stability for fusion while minimizing the extent of instrumentation and surgical exposure. Contemporary construct designs utilize advanced rod materials and connection systems that provide superior fatigue resistance and maintain correction over time. The integration of interbody devices with posterior instrumentation through minimally invasive approaches has become a standard technique for achieving circumferential fusion while limiting surgical morbidity.
Load-sharing principles guide the selection of appropriate implant configurations, with consideration given to the biomechanical demands of each specific spinal level and pathological condition. The ability to achieve three-column spinal stability through strategic implant placement has expanded the indications for minimally invasive surgical approaches to include complex deformity correction and traumatic conditions previously requiring extensive open procedures.
Clinical Applications and Indications
Degenerative Conditions Treatment
Degenerative spinal conditions represent the most common indication for minimally invasive spinal surgery utilizing advanced implant systems. Conditions such as degenerative disc disease, spinal stenosis, and grade I spondylolisthesis have demonstrated excellent outcomes when treated through minimally invasive approaches with appropriate instrumentation. The ability to achieve decompression and fusion through limited surgical exposures has significantly reduced the morbidity associated with treating these common conditions in aging populations.
The treatment of multi-level degenerative conditions through staged minimally invasive procedures has become an effective strategy for managing complex spinal pathology while limiting surgical risk. The use of advanced implant systems enables surgeons to address adjacent level disease through separate surgical episodes, reducing the physiological stress on patients while achieving comprehensive treatment of their spinal pathology. This approach has proven particularly beneficial for elderly patients with multiple comorbidities who may not tolerate extensive single-stage procedures.
Traumatic and Complex Cases
The application of minimally invasive techniques to traumatic spinal injuries has expanded significantly with improvements in implant design and surgical instrumentation. Thoracolumbar burst fractures, flexion-distraction injuries, and certain cervical trauma cases can now be effectively managed through minimally invasive approaches when appropriate patient selection criteria are applied. The ability to achieve immediate spinal stability while minimizing surgical trauma has improved outcomes for polytrauma patients who require rapid mobilization and rehabilitation.
Complex cases involving revision surgery, adjacent segment disease, and pseudarthrosis repair have benefited from minimally invasive approaches that utilize advanced implant systems designed for challenging anatomical situations. The precision afforded by modern guidance systems and specialized instrumentation enables surgeons to address these complex problems while minimizing additional surgical morbidity. The success rates achieved in these challenging cases have expanded the therapeutic options available to patients with complex spinal pathology.
Postoperative Outcomes and Recovery
Enhanced Recovery Protocols
The implementation of enhanced recovery protocols in conjunction with minimally invasive spinal surgery has revolutionized postoperative care and patient rehabilitation timelines. These protocols emphasize early mobilization, optimized pain management strategies, and rapid return to functional activities while maintaining appropriate precautions for fusion healing. The reduced tissue trauma associated with minimally invasive approaches facilitates earlier patient mobilization and shortened hospital stays compared to traditional open procedures.
Multimodal pain management strategies have proven particularly effective in minimally invasive spinal surgery patients, reducing reliance on narcotic medications while maintaining adequate comfort levels during the recovery period. The preservation of muscle attachments and reduced soft tissue dissection contributes significantly to improved pain profiles and faster functional recovery. These factors combine to create a more favorable recovery experience for patients while reducing overall healthcare costs associated with spinal surgery.
Long-term Clinical Results
Long-term clinical studies have demonstrated equivalent or superior outcomes for minimally invasive spinal surgery compared to traditional open approaches across multiple outcome measures. Fusion rates, patient satisfaction scores, and functional improvement indices have consistently shown favorable results for minimally invasive techniques when appropriate patient selection and surgical technique principles are followed. The reduced incidence of adjacent segment disease and revision surgery rates further supports the biological advantages of these surgical approaches.
The preservation of posterior muscular architecture through minimally invasive approaches has demonstrated measurable benefits in long-term functional outcomes, with patients showing improved core strength and spinal mobility compared to those treated through traditional open approaches. These functional advantages translate to improved quality of life measures and higher rates of return to pre-injury activity levels. The combination of effective spinal stabilization with preserved anatomical function represents the optimal outcome for spinal surgery patients.
Future Developments and Innovations
Technology Integration Advances
The future of minimally invasive spinal surgery continues to evolve with advancing technology integration, including robotic-assisted surgery systems, augmented reality visualization, and artificial intelligence-guided surgical planning. These technologies promise to further improve surgical precision while reducing the technical demands on surgeons performing complex minimally invasive procedures. The integration of real-time biomechanical feedback systems may enable optimization of construct design and implant placement during surgery.
Advanced imaging technologies, including intraoperative CT and MRI systems, are being integrated into surgical suites to provide unprecedented visualization of spinal anatomy during minimally invasive procedures. These imaging modalities enable real-time assessment of decompression adequacy, implant positioning, and construct integrity before surgical conclusion. The combination of these imaging advances with minimally invasive surgical techniques represents the next evolution in spinal surgery technology.
Implant Design Evolution
Future implant designs are incorporating smart materials and bioactive coatings that promote accelerated fusion while providing real-time feedback regarding implant integration and construct stability. These advanced materials may include shape-memory alloys that optimize construct configuration based on physiological loading patterns and bioactive surfaces that promote enhanced osseointegration. The development of biodegradable components that provide temporary support during fusion healing represents another promising avenue for implant innovation.
The miniaturization of implant designs while maintaining biomechanical strength continues to drive innovation in spinal instrumentation development. Ultra-low-profile designs that minimize soft tissue irritation while providing adequate stability are being developed for specific clinical applications. These advances promise to further reduce surgical morbidity while expanding the indications for minimally invasive spinal surgery across diverse patient populations and pathological conditions.
FAQ
What advantages do spine screws offer in minimally invasive procedures compared to traditional open surgery
Spine screws designed for minimally invasive procedures provide superior accuracy through navigation guidance while reducing muscle damage and blood loss. The specialized designs enable precise placement through small incisions, resulting in faster recovery times, reduced postoperative pain, and lower infection rates. These implants maintain the same biomechanical stability as traditional approaches while significantly reducing surgical trauma to surrounding tissues.
How long does recovery typically take after minimally invasive spinal surgery with spine screws
Recovery timelines for minimally invasive spinal surgery are significantly shorter than traditional open procedures, with most patients returning to light activities within 2-4 weeks and full activities within 6-12 weeks depending on the extent of surgery. The preserved muscle architecture and reduced tissue trauma contribute to faster healing and rehabilitation. Hospital stays are typically 1-2 days compared to 3-5 days for open procedures, with many patients eligible for same-day discharge in appropriate cases.
Are there specific patient criteria that determine candidacy for minimally invasive spine surgery
Patient candidacy depends on several factors including the specific spinal condition, anatomical considerations, bone quality, and overall health status. Ideal candidates have well-defined pathology amenable to targeted treatment, adequate bone density for implant fixation, and realistic expectations regarding outcomes. Age is not typically a limiting factor, though patients with severe obesity, extensive scarring from previous surgery, or complex deformities may require traditional open approaches for optimal outcomes.
What are the long-term success rates for spine screws in minimally invasive spinal fusion
Long-term success rates for minimally invasive spinal fusion with modern spine screws consistently demonstrate fusion rates exceeding 95% at two years post-surgery with appropriate patient selection. Patient satisfaction scores typically range from 85-95% across multiple outcome measures, with low rates of implant-related complications or revision surgery. The preserved anatomical structures contribute to sustained functional improvement and reduced adjacent segment disease compared to traditional open approaches, supporting excellent long-term clinical results.
Table of Contents
- Fundamental Principles of Minimally Invasive Spinal Surgery
- Biomechanical Engineering of Modern Spinal Implants
- Surgical Technique Considerations
- Clinical Applications and Indications
- Postoperative Outcomes and Recovery
- Future Developments and Innovations
-
FAQ
- What advantages do spine screws offer in minimally invasive procedures compared to traditional open surgery
- How long does recovery typically take after minimally invasive spinal surgery with spine screws
- Are there specific patient criteria that determine candidacy for minimally invasive spine surgery
- What are the long-term success rates for spine screws in minimally invasive spinal fusion

