Modern orthopedic surgery has revolutionized the treatment of bone fractures and skeletal injuries through advanced fixation techniques. Among the most critical innovations in this field are bone plates, which serve as essential tools for providing mechanical stability during the healing process. These specialized medical devices have transformed patient outcomes by offering reliable fracture fixation while promoting optimal bone regeneration. The strategic application of bone plates represents a cornerstone of contemporary trauma surgery, enabling surgeons to address complex fractures that would otherwise compromise patient mobility and quality of life.
Understanding Bone Plate Technology and Design Principles
Material Composition and Biocompatibility Standards
The development of modern bone plates relies heavily on advanced metallurgy and biocompatible materials that ensure long-term integration with human bone tissue. Titanium alloys, particularly Ti-6Al-4V, represent the gold standard in bone plate manufacturing due to their exceptional strength-to-weight ratio and corrosion resistance. These materials exhibit excellent biocompatibility, minimizing the risk of adverse tissue reactions while providing the mechanical properties necessary for effective fracture stabilization. Stainless steel variants, though less commonly used today, continue to play a role in specific applications where cost considerations are paramount.
Surface treatments and coatings further enhance the performance characteristics of bone plates by promoting osseointegration and reducing bacterial adhesion. Plasma-sprayed titanium surfaces create micro-textures that encourage bone cell attachment and proliferation, while specialized antimicrobial coatings help prevent surgical site infections. The careful selection of materials and surface modifications directly impacts the success rate of bone plate implementations, making material science a critical component of orthopedic device development.
Geometric Design and Mechanical Engineering
The geometric configuration of bone plates plays a fundamental role in their ability to provide stable fracture fixation while accommodating the complex loading patterns experienced by different skeletal regions. Anatomical contouring ensures that plates conform to the natural curvature of bones, reducing stress concentrations and improving load distribution across the fracture site. Variable thickness profiles allow engineers to optimize strength where maximum load bearing is required while minimizing bulk in areas where soft tissue coverage is limited.
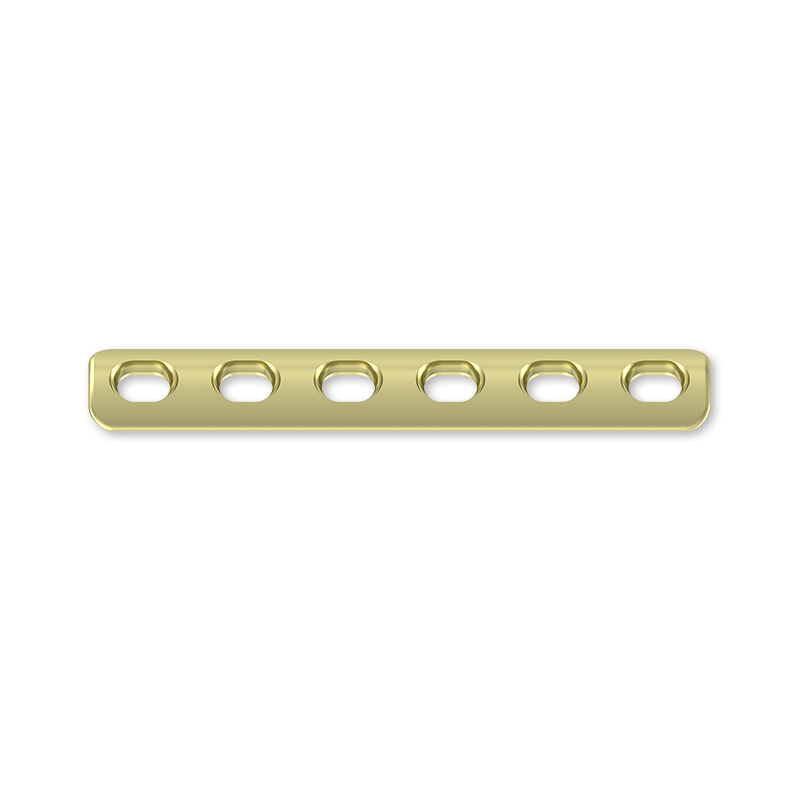
Hole patterns and screw configurations represent another critical aspect of bone plate design, with locking mechanisms providing enhanced stability compared to conventional compression plates. Angular stability achieved through threaded screw heads prevents screw loosening and maintains fracture reduction throughout the healing period. The strategic placement of screw holes enables surgeons to customize fixation patterns based on fracture morphology and patient-specific anatomical considerations.
Clinical Applications and Surgical Techniques
Fracture Classification and Treatment Planning
Successful implementation of bone plates requires comprehensive understanding of fracture patterns and appropriate surgical planning methodologies. Complex fractures involving multiple fragments demand careful analysis to determine optimal plate positioning and screw trajectory planning. Surgeons must evaluate bone quality, fracture stability, and soft tissue condition when selecting appropriate plate configurations. The AO classification system provides standardized criteria for fracture assessment, guiding treatment decisions and plate selection protocols.
Preoperative imaging studies, including CT scans and three-dimensional reconstructions, enable precise surgical planning and template preparation. Digital templating software allows surgeons to virtually position bone plates and simulate screw placement before entering the operating room. This advanced planning reduces surgical time and improves the accuracy of implant positioning, ultimately leading to better patient outcomes and reduced complication rates.
Minimally Invasive Surgical Approaches
Contemporary surgical techniques emphasize minimally invasive approaches that preserve soft tissue integrity while achieving stable fracture fixation. Percutaneous plating techniques utilize small incisions and specialized instrumentation to position bone plates with minimal soft tissue disruption. These approaches maintain the biological environment around fracture sites, promoting faster healing and reducing the risk of complications such as infection and delayed union.
Bridge plating concepts represent another advancement in minimally invasive fracture treatment, where plates span comminuted fracture zones without direct manipulation of bone fragments. This technique preserves the fracture hematoma and maintains blood supply to bone fragments, creating optimal conditions for biological healing. Indirect reduction techniques combined with appropriate plate positioning achieve mechanical stability while respecting the biological principles of fracture healing.

Biomechanical Advantages and Healing Enhancement
Load Distribution and Stress Management
The primary biomechanical advantage of bone plates lies in their ability to redistribute mechanical loads across fracture sites while maintaining anatomical alignment during the healing process. Proper plate application converts unstable fracture patterns into stable constructs capable of withstanding physiological loading conditions. The principle of load sharing between the plate and healing bone ensures that mechanical forces are gradually transferred back to the regenerating tissue as healing progresses.
Stress shielding represents a critical consideration in bone plate design, as overly rigid implants can lead to bone resorption and weakening of the underlying skeletal structure. Modern plate designs incorporate controlled flexibility that allows appropriate mechanical stimulation of healing bone while providing necessary stability. The balance between stability and flexibility remains a key engineering challenge in developing next-generation bone plate systems.
Biological Healing Enhancement Mechanisms
Beyond mechanical stabilization, bone plates contribute to healing enhancement through several biological mechanisms that promote optimal bone regeneration. Stable fixation eliminates interfragmentary motion that could disrupt the formation of callus tissue and delay the healing process. The maintenance of proper fracture alignment ensures that bone formation occurs along anatomically correct pathways, preventing malunion and associated functional impairments.
Compression plating techniques can actively promote healing by applying controlled compressive forces across fracture lines, stimulating bone formation through mechanotransduction pathways. Primary bone healing occurs when anatomical reduction is combined with absolute stability, while secondary healing with callus formation is encouraged in situations where some degree of motion is beneficial. The ability to control healing mechanics through appropriate plate selection and application techniques represents a significant advantage in modern fracture treatment.
Long-term Outcomes and Patient Benefits
Functional Recovery and Quality of Life Improvements
The implementation of bone plates in fracture treatment has dramatically improved functional outcomes and patient quality of life compared to historical treatment methods. Early mobilization protocols enabled by stable plate fixation prevent joint stiffness and muscle atrophy that commonly occur with prolonged immobilization. Patients can often begin range-of-motion exercises and partial weight-bearing activities within days of surgery, accelerating the overall recovery process.
Long-term follow-up studies demonstrate that patients treated with appropriately selected and positioned bone plates achieve superior functional scores compared to those managed with conservative methods or alternative fixation techniques. Return to work and recreational activities occurs significantly earlier, with reduced risk of chronic pain and disability. The psychological benefits of early mobility and faster recovery contribute substantially to overall patient satisfaction and well-being.
Complication Prevention and Management Strategies
Modern bone plate systems have significantly reduced the incidence of complications associated with fracture treatment, though careful attention to surgical technique and postoperative management remains essential. Infection prevention protocols, including antibiotic prophylaxis and sterile surgical techniques, have minimized the risk of implant-related infections. When complications do occur, the modular design of contemporary plate systems often allows for revision procedures without complete implant removal.
Hardware-related complications such as screw loosening, plate breakage, or implant prominence can be effectively managed through appropriate patient selection and surgical technique refinement. The development of anatomically pre-contoured plates has reduced the need for intraoperative bending, minimizing stress concentrations that could lead to implant failure. Regular follow-up monitoring and patient education regarding activity restrictions help prevent complications while promoting optimal healing outcomes.
Future Developments and Technological Innovations
Smart Implant Technologies and Monitoring Systems
The future of bone plate technology lies in the development of smart implant systems that incorporate sensors and monitoring capabilities to provide real-time feedback on healing progress and mechanical loading conditions. Embedded strain gauges and accelerometers could enable continuous assessment of implant performance and bone healing status, allowing for personalized rehabilitation protocols and early detection of potential complications.
Wireless communication technologies integrated into bone plates could transmit data to external monitoring devices, creating comprehensive digital health records that track patient progress throughout the healing process. Machine learning algorithms applied to this data could identify patterns predictive of successful outcomes or potential complications, enabling proactive interventions and optimized treatment protocols. These technological advances represent the next frontier in personalized orthopedic care.
Biodegradable and Bioresorbable Plate Systems
Research into biodegradable bone plates represents a paradigm shift toward temporary fixation devices that eliminate the need for implant removal procedures. Polymer-based materials such as polylactic acid and polyglycolic acid offer controlled degradation rates that can be matched to bone healing timelines. These materials gradually transfer load back to healing bone as they degrade, potentially reducing long-term complications associated with permanent implants.
Composite materials combining biodegradable polymers with bioactive ceramics or growth factors could enhance healing while providing temporary mechanical support. The ability to customize degradation rates and mechanical properties through material engineering offers exciting possibilities for patient-specific treatment approaches. Clinical trials of biodegradable bone plates show promising results, though long-term outcome data continues to be collected to validate their effectiveness compared to traditional metallic implants.
FAQ
How long do bone plates typically remain in the body after surgery
Bone plates are generally designed as permanent implants that remain in the body indefinitely unless complications arise or removal becomes necessary for specific medical reasons. Most patients do not require plate removal, as modern materials are biocompatible and well-tolerated by the body over long periods. However, removal may be considered in cases of infection, implant prominence causing discomfort, or patient preference, typically occurring 12-18 months after the initial surgery once healing is complete.
What are the main risks and complications associated with bone plate surgery
The primary risks associated with bone plate surgery include infection, nerve or blood vessel injury, implant loosening or breakage, and nonunion or malunion of the fracture. Modern surgical techniques and improved implant designs have significantly reduced these risks, with overall complication rates typically ranging from 5-15% depending on fracture complexity and patient factors. Most complications can be successfully managed with appropriate treatment, and the benefits of stable fracture fixation generally outweigh the potential risks.
Can bone plates be detected by metal detectors or affect medical imaging
Bone plates may trigger metal detectors at airports and security checkpoints, though this varies depending on the size and material of the implant. Patients should carry documentation of their surgical procedure when traveling. Regarding medical imaging, bone plates are clearly visible on X-rays and CT scans, which is actually beneficial for monitoring healing progress. MRI compatibility depends on the implant material, with titanium plates generally being MRI-safe, though some image distortion may occur near the implant site.
How do bone plates affect physical activity and sports participation after healing
Once complete healing has occurred and the surgeon has cleared the patient for full activity, bone plates typically do not significantly restrict physical activity or sports participation. Many professional athletes have successfully returned to high-level competition after bone plate surgery. However, individual recommendations may vary based on fracture location, sport-specific demands, and surgeon preference. Some contact sports may carry increased risk of re-injury, and patients should discuss activity restrictions with their orthopedic surgeon before returning to high-impact activities.