Selecting the appropriate bone plate for fracture repair is a critical decision that significantly impacts patient outcomes and recovery times. Modern orthopedic surgery relies heavily on advanced fixation systems, with bone plates serving as essential tools for stabilizing fractures across various anatomical locations. The choice of bone plate depends on multiple factors including fracture pattern, bone quality, patient age, and the specific biomechanical requirements of the affected area. Understanding these variables ensures optimal surgical outcomes and promotes faster healing while minimizing complications.
The evolution of bone plate technology has revolutionized fracture management, offering surgeons numerous options tailored to specific clinical scenarios. From traditional compression plates to modern locking systems, each design addresses particular biomechanical challenges. Successful fracture repair requires careful consideration of plate geometry, material properties, and fixation mechanisms to achieve stable reduction and promote optimal bone healing. This comprehensive approach to bone plate selection directly influences surgical success rates and patient satisfaction.
Understanding Fracture Classifications and Plate Requirements
Simple Versus Complex Fracture Patterns
Simple fractures typically involve clean breaks with minimal comminution, making them suitable for straightforward bone plate applications. These fractures often respond well to compression plating techniques, where the plate applies direct pressure to maintain bone contact during healing. The selection process focuses on achieving adequate length and screw density to provide sufficient stability without over-engineering the construct.
Complex fractures present greater challenges, often featuring multiple fragments, significant comminution, or segmental bone loss. These cases require specialized bone plate designs that can bridge defects while providing adequate stability for healing. Locking plate systems frequently prove superior in complex scenarios due to their ability to maintain reduction without relying solely on bone-plate interface friction. The angular stability provided by locking mechanisms prevents secondary displacement and supports healing in compromised bone environments.
Anatomical Considerations for Plate Selection
Different anatomical regions present unique biomechanical challenges that influence bone plate selection criteria. Long bone fractures in the femur or tibia require robust plates capable of withstanding significant loading forces during weight-bearing activities. These applications often necessitate broader plates with increased screw density to distribute forces effectively across the bone-plate interface.
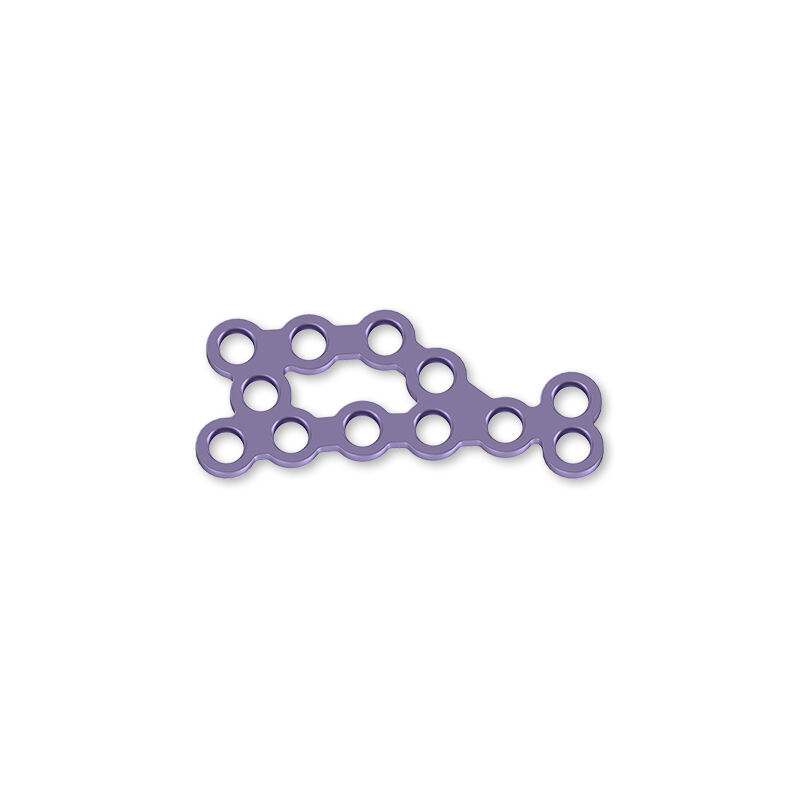
Smaller bones, such as those in the hand or foot, require specialized bone plate designs that accommodate limited soft tissue coverage and reduced bone stock. Thin profile plates with smaller screw diameters provide adequate fixation while minimizing soft tissue irritation and maintaining joint function. The geometric constraints of these anatomical regions often dictate specific plate contours and fixation strategies.
Material Properties and Biocompatibility Factors
Titanium Versus Stainless Steel Options
Titanium alloys have become the gold standard for modern bone plate manufacturing due to their exceptional biocompatibility and favorable mechanical properties. The lower elastic modulus of titanium more closely matches bone tissue, reducing stress shielding effects that can lead to bone resorption around implants. Additionally, titanium's corrosion resistance ensures long-term stability in the biological environment.
Stainless steel bone plates remain viable options for specific applications, particularly in temporary fixation scenarios or when cost considerations are paramount. While offering excellent strength characteristics, stainless steel's higher stiffness may contribute to stress shielding in some applications. The choice between materials often depends on patient-specific factors, expected implant duration, and surgical objectives.
Surface Treatments and Osseointegration
Modern bone plate surfaces undergo specialized treatments to enhance osseointegration and reduce infection risk. Anodized surfaces provide improved corrosion resistance while promoting favorable tissue responses. Some manufacturers incorporate antimicrobial coatings or surface modifications that encourage bone ingrowth around the implant periphery.
The surface roughness of bone plates influences cellular attachment and subsequent bone formation. Controlled surface textures promote osteoblast adhesion while discouraging bacterial colonization. These surface engineering advances contribute significantly to improved clinical outcomes and reduced complication rates in fracture repair procedures.
Locking Versus Non-Locking Plate Systems
Compression Plating Mechanisms
Traditional compression plates rely on friction between the plate and bone surface to maintain fracture reduction. These systems excel in simple fracture patterns with good bone quality, where direct compression can promote primary bone healing. The technique requires careful pre-contouring and precise application to achieve optimal compression without over-reduction.
Compression plating techniques work best when adequate bone stock exists on both sides of the fracture site. The success of these systems depends heavily on proper surgical technique and post-operative compliance with weight-bearing restrictions. When applied correctly, compression plates can achieve excellent outcomes in appropriate cases while maintaining relatively simple surgical procedures.
Angular Stability in Locking Systems
Locking bone plate systems provide angular stability through threaded screw-plate interfaces, creating fixed-angle constructs that function as internal external fixators. This design eliminates reliance on bone-plate friction and proves particularly valuable in osteoporotic bone or comminuted fractures where traditional fixation might fail.
The versatility of locking systems allows for various screw configurations, including combinations of locking and non-locking screws within the same construct. This flexibility enables surgeons to optimize fixation strategies based on local bone quality and fracture characteristics. bone plate systems with locking capabilities have expanded treatment options for previously challenging fracture patterns.
Size Selection and Geometric Considerations
Length and Width Optimization
Proper bone plate length selection ensures adequate fracture stability while minimizing unnecessary hardware exposure. The general principle involves spanning the fracture zone with sufficient plate length to accommodate at least three screws on each side of the fracture. This configuration provides redundancy in case of individual screw failure while distributing forces over an appropriate bone segment.
Plate width must accommodate the anatomical constraints of the surgical site while providing adequate structural strength. Wider plates offer increased resistance to bending forces but may present challenges in areas with limited soft tissue coverage. The balance between structural adequacy and biological compatibility guides optimal width selection for each clinical scenario.
Thickness and Profile Considerations
Plate thickness directly influences both mechanical strength and biological impact on surrounding tissues. Thicker plates provide greater resistance to fatigue failure but may increase soft tissue irritation and complicate future hardware removal procedures. Modern design philosophy emphasizes optimized thickness that provides adequate strength while minimizing biological disruption.
Low-profile bone plate designs have gained popularity due to their reduced impact on surrounding soft tissues. These systems maintain structural integrity through advanced metallurgy and geometric optimization rather than simply increasing material thickness. The result is improved patient comfort and reduced complication rates without compromising mechanical performance.
Specific Applications in Common Fracture Types
Long Bone Fracture Management
Femoral and tibial fractures represent common applications for bone plate fixation, particularly in cases where intramedullary nailing is contraindicated or inappropriate. These applications typically require robust plate systems capable of withstanding significant physiological loads while maintaining fracture alignment during healing.
The selection process for long bone plates considers factors such as patient activity level, bone quality, and fracture complexity. High-demand patients may require reinforced plate designs or augmented fixation strategies to prevent hardware failure during the healing period. Conversely, elderly patients with limited mobility may benefit from less robust but more biologically friendly implant systems.
Periarticular Fracture Considerations
Fractures near joints present unique challenges due to complex geometry and the need to preserve joint function. Specialized bone plate designs for periarticular applications often feature variable screw angles and anatomically contoured profiles that accommodate joint capsule attachments and ligament insertions.
The proximity to articular surfaces requires careful attention to plate positioning and screw trajectory to avoid joint penetration or interference with normal joint mechanics. Pre-contoured plates designed for specific anatomical regions help surgeons achieve optimal positioning while reducing operative time and improving reproducibility of results.
Surgical Technique and Plate Positioning
Approach Selection and Soft Tissue Management
The surgical approach for bone plate application significantly influences both immediate and long-term outcomes. Minimally invasive techniques reduce soft tissue disruption and preserve the biological environment around the fracture site. These approaches require specialized instrumentation and careful pre-operative planning to ensure adequate plate positioning and screw placement.
Traditional open approaches provide excellent visualization and direct fracture manipulation but may compromise soft tissue vitality around the implant. The choice between approaches depends on fracture complexity, surgeon experience, and available instrumentation. Regardless of approach, careful soft tissue handling and meticulous closure techniques minimize complications and promote optimal healing.
Screw Placement Strategies
Optimal screw placement maximizes bone purchase while avoiding critical structures such as neurovascular bundles and joint surfaces. The distribution of screws along the bone plate length should provide balanced support without creating stress concentrations that might lead to implant failure or bone fracture.
Modern imaging techniques and computer-assisted navigation systems help surgeons achieve precise screw placement, particularly in complex anatomical regions. These technologies reduce the risk of malposition and improve overall construct quality. The investment in advanced surgical techniques often translates to improved patient outcomes and reduced complication rates.
Complications and Troubleshooting
Hardware-Related Complications
Bone plate complications can include infection, hardware loosening, breakage, and soft tissue irritation. Early recognition and appropriate management of these complications prevent more serious sequelae and preserve treatment options. Regular follow-up examinations and imaging studies help identify problems before they become severe.
Prevention strategies focus on proper patient selection, meticulous surgical technique, and appropriate post-operative care protocols. Understanding the biomechanical limitations of different bone plate systems helps surgeons avoid overloading constructs and reduces the risk of hardware failure. Patient education regarding activity restrictions and warning signs plays a crucial role in complication prevention.
Revision Surgery Considerations
When bone plate complications occur, revision surgery may become necessary to preserve limb function and patient quality of life. The approach to revision depends on the specific complication, remaining bone stock, and patient factors such as age and activity level. Planning for potential revision scenarios during initial surgery can simplify future procedures if needed.
Removal of bone plates after successful healing remains a topic of debate in orthopedic surgery. Factors favoring removal include patient age, activity level, and symptoms related to hardware presence. Conversely, successful integration and absence of symptoms may support leaving implants in place to avoid unnecessary surgical risks.
FAQ
What factors determine the appropriate bone plate size for a specific fracture
The appropriate bone plate size depends on several key factors including fracture location, bone diameter, fracture pattern complexity, and patient-specific characteristics such as age and activity level. Generally, the plate should span the fracture with at least three screw holes on each side of the break, providing adequate stability while minimizing unnecessary hardware. Bone quality, particularly in elderly patients with osteoporosis, may require longer plates with more screws to distribute forces effectively and prevent fixation failure.
How do locking plates differ from traditional compression plates in terms of application
Locking plates create angular stability through threaded screw-plate interfaces, functioning like internal external fixators that don't rely on bone-plate compression for stability. This makes them ideal for osteoporotic bone, comminuted fractures, and situations where achieving adequate compression is difficult. Traditional compression plates work through friction between the plate and bone surface, requiring good bone quality and proper technique to achieve compression across the fracture site.
What are the most common complications associated with bone plate fixation
Common complications include infection, hardware loosening or breakage, soft tissue irritation, and delayed union or nonunion of the fracture. Infection rates vary but typically range from 2-5% in closed fractures and higher in open fractures. Hardware complications may result from improper sizing, poor surgical technique, or patient non-compliance with activity restrictions. Early recognition through regular follow-up and imaging studies allows for timely intervention when complications arise.
When should bone plates be removed after successful fracture healing
Bone plate removal decisions depend on patient age, symptoms, activity level, and implant-related complications. Younger patients with symptomatic hardware or those engaged in high-impact activities may benefit from removal once healing is complete. However, successful integration without symptoms often supports leaving plates in place to avoid surgical risks. The decision should be individualized based on patient preferences, symptoms, and surgeon assessment of risks versus benefits of removal surgery.
Table of Contents
- Understanding Fracture Classifications and Plate Requirements
- Material Properties and Biocompatibility Factors
- Locking Versus Non-Locking Plate Systems
- Size Selection and Geometric Considerations
- Specific Applications in Common Fracture Types
- Surgical Technique and Plate Positioning
- Complications and Troubleshooting
-
FAQ
- What factors determine the appropriate bone plate size for a specific fracture
- How do locking plates differ from traditional compression plates in terms of application
- What are the most common complications associated with bone plate fixation
- When should bone plates be removed after successful fracture healing

