Maxillofacial surgery has evolved significantly over the past few decades, with advanced fixation systems playing a crucial role in improving patient outcomes. Modern surgical practices increasingly rely on specialized implants and devices to ensure proper healing and functional restoration. Among these innovations, maxillofacial plates have emerged as essential components in reconstructive and corrective procedures involving the facial skeleton. These titanium-based devices provide critical support during the healing process, enabling surgeons to achieve more predictable results while minimizing complications and reducing recovery time for patients undergoing complex facial surgeries.
Understanding Maxillofacial Plate Technology
Material Composition and Biocompatibility
The development of maxillofacial plates represents a significant advancement in biomaterial engineering. These devices are typically manufactured from medical-grade titanium or titanium alloys, materials chosen for their exceptional biocompatibility and corrosion resistance. The surface treatment processes applied to these plates enhance osseointegration, allowing bone tissue to grow directly onto the implant surface. This integration creates a stable foundation for long-term functional restoration and reduces the risk of implant loosening or migration over time.
Modern manufacturing techniques ensure that each plate maintains precise dimensional tolerances while exhibiting optimal mechanical properties. The titanium construction provides an ideal balance between strength and flexibility, allowing the plates to withstand the complex forces generated during normal facial function. Advanced surface modifications, including anodization and plasma spraying, further enhance the biological response and promote faster healing around the implant site.
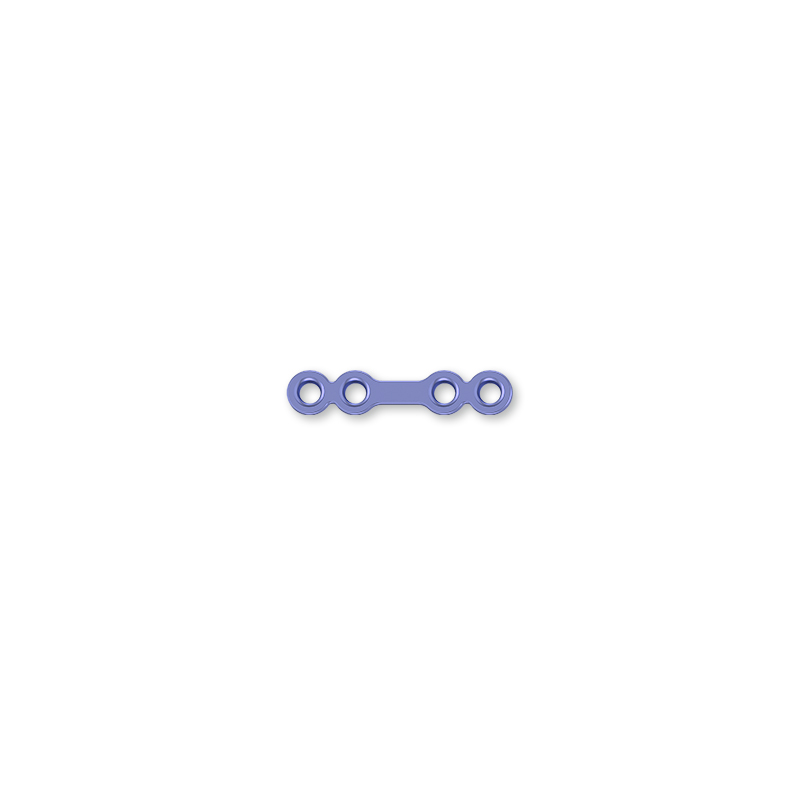
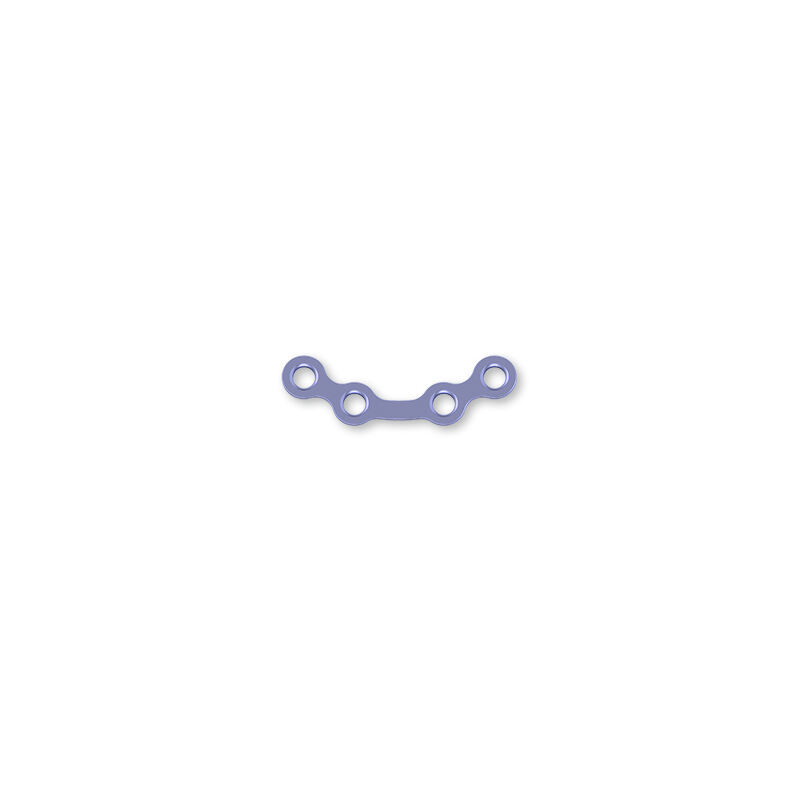
Design Innovations and Anatomical Considerations
Contemporary maxillofacial plates feature sophisticated design elements that accommodate the complex three-dimensional anatomy of the facial skeleton. Manufacturers utilize advanced computer modeling and anatomical studies to develop plate configurations that match the natural contours of different facial regions. These anatomically contoured designs reduce the need for intraoperative bending, minimizing surgical time and improving the precision of reconstruction.
The incorporation of low-profile designs has revolutionized patient comfort and aesthetic outcomes. Thinner plate profiles reduce palpability through the soft tissues while maintaining structural integrity. Strategic placement of screw holes allows surgeons to achieve optimal fixation without interfering with critical anatomical structures such as nerve pathways or dental roots. These design refinements have significantly expanded the applications for maxillofacial plates across various surgical specialties.
Clinical Applications and Surgical Benefits
Trauma Reconstruction and Emergency Procedures
In emergency trauma situations, maxillofacial plates serve as critical tools for restoring facial skeletal continuity and function. High-energy impacts from motor vehicle accidents, sports injuries, or interpersonal violence often result in complex fracture patterns that require immediate surgical intervention. These plates provide reliable fixation for mandibular fractures, orbital floor defects, and zygomatic complex injuries, enabling surgeons to restore normal facial anatomy even in severely compromised cases.
The use of rigid internal fixation with maxillofacial plates has largely replaced traditional methods such as intermaxillary fixation and external fixation devices. This advancement allows patients to maintain normal jaw function during healing, reducing complications associated with prolonged immobilization. Early mobilization protocols supported by stable plate fixation contribute to improved functional outcomes and faster return to normal activities.
Orthognathic Surgery and Corrective Procedures
Orthognathic surgery relies heavily on precise positioning and stable fixation of bone segments to achieve optimal functional and aesthetic results. Maxillofacial plates provide the mechanical stability necessary for successful bone healing in predetermined positions. During complex jaw repositioning procedures, these plates maintain the surgical correction while allowing controlled loading during the healing phase.
The versatility of maxillofacial plates enables surgeons to address various deformities including mandibular prognathism, retrognathia, and asymmetries. Pre-surgical planning using three-dimensional imaging allows for precise plate selection and positioning strategies. This technological integration has significantly improved the predictability of surgical outcomes while reducing the need for revision procedures.
Impact on Patient Recovery and Outcomes
Accelerated Healing Processes
The implementation of maxillofacial plates in surgical protocols has demonstrated measurable improvements in healing timelines and patient recovery metrics. Stable mechanical fixation provided by these devices creates an optimal environment for bone regeneration and soft tissue healing. The reduced micromotion at fracture sites promotes primary bone healing, which is faster and more predictable than secondary healing processes.
Clinical studies consistently show that patients treated with appropriate plate fixation experience shorter hospital stays and reduced pain levels compared to traditional treatment methods. The ability to resume normal oral function immediately following surgery contributes to improved nutritional status and overall patient satisfaction. These factors collectively result in faster return to work and normal social activities, providing significant quality of life benefits.
Long-Term Functional Restoration
Long-term follow-up studies demonstrate that maxillofacial plates contribute to sustained functional improvements across multiple parameters. Patients maintain better occlusal relationships, improved masticatory efficiency, and enhanced facial symmetry when compared to alternative treatment approaches. The durability of titanium construction ensures that these benefits persist throughout the patient's lifetime without degradation of implant performance.
The biocompatible nature of modern maxillofacial plates minimizes the risk of adverse tissue reactions or implant-related complications. Long-term osseointegration creates a permanent biological bond that actually strengthens over time. This integration eliminates the need for plate removal in most cases, reducing patient morbidity and healthcare costs associated with secondary procedures.
Selection Criteria and Surgical Considerations
Patient-Specific Factors and Assessment
Successful implementation of maxillofacial plates requires careful evaluation of patient-specific factors including bone quality, age, medical history, and expected functional demands. Surgeons must assess the mechanical requirements for each case, considering factors such as bite forces, bone healing capacity, and anatomical constraints. Preoperative imaging studies provide critical information for selecting appropriate plate dimensions and configurations.
Patient counseling regarding the permanent nature of implanted devices and potential long-term considerations forms an essential component of the surgical planning process. Understanding patient expectations and lifestyle factors helps surgeons optimize treatment recommendations and improve overall satisfaction with surgical outcomes. Comprehensive preoperative assessment ensures that maxillofacial plates are utilized in appropriate clinical scenarios where maximum benefit can be achieved.
Surgical Technique and Placement Strategies
Optimal surgical outcomes with maxillofacial plates depend on meticulous attention to technique and adherence to established placement principles. Proper plate contouring, appropriate screw selection, and accurate positioning relative to anatomical landmarks are critical factors determining long-term success. Surgeons must balance mechanical requirements with biological considerations to achieve stable fixation without compromising surrounding tissues.
Intraoperative verification of plate position using imaging guidance helps ensure accurate placement and reduces the risk of complications. The development of computer-assisted surgical planning has further enhanced precision in plate positioning, allowing surgeons to virtually plan procedures and predict outcomes before entering the operating room. These technological advances continue to improve the reliability and predictability of maxillofacial plate applications.
FAQ
How long do maxillofacial plates remain in the body
Maxillofacial plates are designed as permanent implants that typically remain in place for the patient's lifetime. The titanium construction and biocompatible surface treatments ensure long-term stability and integration with surrounding bone tissue. Removal is only considered in rare cases involving infection, mechanical complications, or patient-specific factors that require surgical intervention. Most patients experience no issues with permanent plate retention and benefit from continued structural support throughout their lives.
What are the potential risks associated with maxillofacial plate surgery
As with any surgical procedure, maxillofacial plate implantation carries certain risks including infection, bleeding, nerve damage, and anesthetic complications. Specific to plate surgery, potential issues may include implant loosening, screw breakage, or plate exposure through the overlying soft tissues. However, these complications occur infrequently when proper surgical technique is employed and appropriate patient selection criteria are followed. Modern surgical protocols and improved implant designs have significantly reduced complication rates compared to earlier generation devices.
Can maxillofacial plates be detected by airport security systems
Titanium maxillofacial plates may occasionally trigger metal detectors at airport security checkpoints, although this occurrence is relatively uncommon due to the small amount of metal involved. Patients with implanted plates should carry documentation from their surgeon describing the medical devices to facilitate security screening if questions arise. Most modern security systems are calibrated to minimize false alarms from medical implants, and trained security personnel are familiar with handling these situations professionally and efficiently.
Do maxillofacial plates require special care or maintenance
Maxillofacial plates require no special maintenance or care once properly integrated following surgery. Patients can resume normal oral hygiene practices, dietary habits, and physical activities without restrictions related to the implanted device. Regular dental and medical checkups allow healthcare providers to monitor the healing process and long-term stability of the plates. The inert nature of titanium construction means that the plates do not deteriorate over time and maintain their mechanical properties indefinitely under normal physiological conditions.