Orthopedic surgeons face critical decisions when treating long bone fractures, particularly in determining the most effective stabilization method. Among the various internal fixation techniques available, intramedullary nails have emerged as a gold standard for specific fracture patterns and patient populations. Understanding when these specialized implants provide optimal outcomes requires comprehensive knowledge of fracture mechanics, patient factors, and surgical considerations that influence treatment success.
The selection of appropriate fixation methods directly impacts patient recovery time, functional outcomes, and long-term quality of life. Modern orthopedic practice relies on evidence-based protocols that consider multiple variables including fracture location, bone quality, patient age, and activity level. Surgeons must evaluate each case individually to determine whether intramedullary nailing offers advantages over alternative treatments such as plate fixation, external fixation, or conservative management.
Fracture Types Best Suited for Intramedullary Nailing
Diaphyseal Fractures of Long Bones
Shaft fractures of the femur, tibia, and humerus represent the primary indications for intramedullary nails due to the biomechanical advantages these devices provide. The central placement of the nail within the medullary canal creates an optimal load-sharing environment that closely mimics normal bone mechanics. This positioning allows for early weight-bearing and mobilization, which are crucial factors in preventing complications such as muscle atrophy, joint stiffness, and deep vein thrombosis.
Femoral shaft fractures particularly benefit from intramedullary fixation because of the high mechanical stresses the femur experiences during normal activities. The nail's position along the bone's neutral axis minimizes bending moments and provides superior resistance to rotational forces compared to extramedullary implants. Clinical studies consistently demonstrate faster healing times and lower complication rates when treating femoral diaphyseal fractures with appropriate nail systems.
Comminuted and Segmental Fractures
Complex fracture patterns with multiple bone fragments present unique challenges that intramedullary nails address effectively. The nail acts as an internal splint that maintains length and alignment while allowing controlled motion at the fracture site, promoting callus formation through beneficial mechanical stimulation. Unlike plate fixation, which requires extensive soft tissue dissection and may compromise the blood supply to bone fragments, intramedullary nailing preserves the fracture hematoma and periosteal circulation.
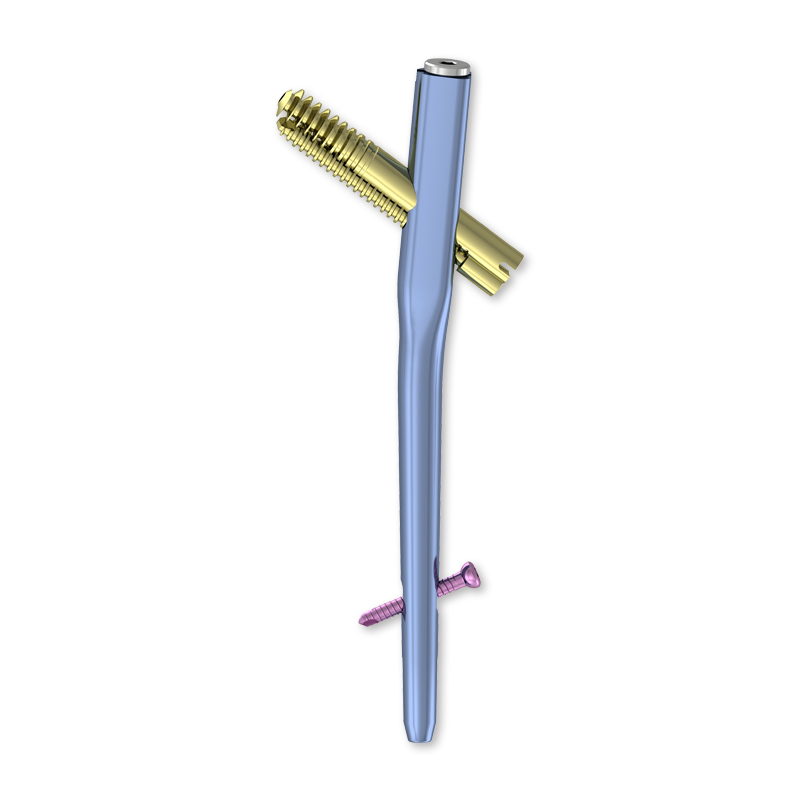
Segmental fractures, where the bone is broken into three or more major pieces, benefit from the nail's ability to stabilize multiple fracture levels simultaneously. The continuous support provided by the intramedullary device prevents shortening and maintains proper limb length, which is particularly important for functional outcomes. Modern locking nail systems offer additional stability through proximal and distal interlocking screws that prevent rotation and translation at fracture sites.
Patient-Specific Considerations for Nail Selection
Age and Activity Level Factors
Younger, more active patients typically benefit most from intramedullary nailing due to their higher functional demands and greater healing potential. The biomechanical advantages of central nail placement allow these patients to return to demanding activities more quickly and with better long-term outcomes. Bone quality in younger individuals also provides superior purchase for locking screws and better integration with the implant surface.
Elderly patients present different considerations, as osteoporotic bone may not provide adequate fixation strength for standard locking mechanisms. However, specialized nail designs with enhanced proximal fixation options, such as helical blades or multiple locking screws, can address these challenges effectively. The reduced soft tissue trauma associated with intramedullary techniques often results in faster recovery and fewer wound complications in older patients compared to more extensive surgical approaches.
Bone Quality and Anatomical Variations
Bone density measurements and canal morphology significantly influence the success of intramedullary fixation. Patients with adequate cortical thickness and normal medullary canal dimensions are ideal candidates for standard nail systems. Preoperative imaging studies help determine canal diameter, bow, and any anatomical variations that might complicate nail insertion or affect final positioning.
Metabolic bone diseases, previous infections, or congenital abnormalities may contraindicate intramedullary nailing in certain cases. Surgeons must carefully evaluate each patient's bone quality through dual-energy X-ray absorptiometry when available, or assess cortical thickness on standard radiographs. Poor bone quality may necessitate alternative fixation methods or specialized implant designs with enhanced anchoring mechanisms.

Biomechanical Advantages of Intramedullary Systems
Load Distribution and Stress Transfer
The central placement of intramedullary nails creates an optimal mechanical environment for fracture healing by distributing loads along the bone's natural axis. This positioning minimizes stress concentrations that can occur with eccentric plate placement and reduces the risk of implant failure under physiological loading conditions. The nail acts as a flexible internal splint that allows controlled micro-motion at the fracture site, which research has shown to promote callus formation and accelerate healing.
Finite element analyses demonstrate that intramedullary fixation produces more uniform stress distribution across the fracture zone compared to other fixation methods. This biomechanical advantage translates to clinical benefits including reduced healing times, lower rates of delayed union, and decreased incidence of hardware failure. The load-sharing characteristics of nail fixation also help prevent the stress shielding effects that can occur with rigid plate constructs.
Preservation of Biological Environment
Minimally invasive insertion techniques for intramedullary nails preserve the fracture site's biological environment, maintaining the natural healing cascade that begins immediately after injury. The nail can be inserted through small incisions away from the fracture zone, avoiding disruption of the periosteal blood supply and the fracture hematoma that contains essential growth factors and healing mediators.
This biological preservation is particularly important in comminuted fractures where maintaining blood supply to bone fragments is crucial for healing. Unlike open reduction and plate fixation, which requires extensive soft tissue dissection and direct fracture manipulation, closed nailing techniques allow fractures to heal in their natural biological environment with minimal surgical trauma.
Comparative Analysis with Alternative Fixation Methods
Advantages Over Plate Fixation
Intramedullary nails offer several significant advantages over plate fixation systems in appropriate cases. The reduced soft tissue dissection required for nail insertion results in less surgical trauma, decreased blood loss, and lower infection rates. Patients typically experience less postoperative pain and faster recovery times due to the minimally invasive nature of the procedure.
The biomechanical superiority of intramedullary fixation becomes apparent when comparing stress distribution patterns and failure modes. Plates create stress concentrations at screw holes and can lead to cortical bone weakening beneath the implant. Nails distribute loads more evenly and maintain the bone's natural flexibility, reducing the risk of refracture after implant removal.
Limitations and Contraindications
Despite their advantages, intramedullary nails are not suitable for all fracture patterns and patient populations. Metaphyseal fractures, particularly those involving joint surfaces, typically require different fixation strategies that can address articular reconstruction needs. Fractures in locations with narrow or abnormal medullary canals may not accommodate standard nail designs safely.
Certain patient factors also contraindicate intramedullary nailing, including active infections at the fracture site, severe osteoporosis that prevents adequate fixation, and anatomical abnormalities that preclude safe nail insertion. Open fractures with significant contamination may require staged treatment protocols that initially utilize external fixation before definitive intramedullary stabilization.
Modern Technological Advances in Nail Design
Enhanced Locking Mechanisms
Contemporary intramedullary nail systems incorporate sophisticated locking mechanisms that provide superior rotational and axial stability compared to earlier designs. Multi-directional locking options allow surgeons to customize fixation based on specific fracture patterns and bone quality. Angular stable locking screws create fixed-angle constructs that resist toggle and maintain reduction even in osteoporotic bone.
Compression capabilities integrated into modern nail systems enable dynamic compression at the fracture site during healing while maintaining the benefits of intramedullary fixation. These features allow surgeons to optimize the mechanical environment for specific healing phases, promoting both initial stability and later consolidation through controlled loading.
Material Science Improvements
Advances in metallurgy and surface treatments have significantly improved the biocompatibility and performance characteristics of modern intramedullary nails. Titanium alloys provide optimal strength-to-weight ratios while minimizing stress shielding effects through modulus matching with bone tissue. Surface modifications enhance osseointegration and reduce the risk of implant-related complications.
Coating technologies have introduced antimicrobial properties to nail surfaces, reducing infection risks in high-risk patients. These technological improvements have expanded the indications for intramedullary nailing and improved outcomes across diverse patient populations, making these devices increasingly attractive options for complex fracture management.
FAQ
What types of fractures are best treated with intramedullary nails?
Intramedullary nails are most effective for diaphyseal fractures of long bones, particularly the femur and tibia. They excel in treating shaft fractures, comminuted injuries with multiple bone fragments, and segmental fractures where maintaining length and alignment is crucial. The central placement of the nail provides optimal biomechanical support for these fracture patterns.
How do patient age and bone quality affect nail selection decisions?
Younger patients with good bone quality are ideal candidates for standard intramedullary nailing due to superior healing potential and higher functional demands. Elderly patients with osteoporotic bone may require specialized nail designs with enhanced fixation mechanisms. Surgeons must evaluate bone density and cortical thickness to ensure adequate implant stability and appropriate healing outcomes.
What are the main advantages of intramedullary nails compared to plate fixation?
Intramedullary nails offer superior biomechanical properties through central load distribution, require less soft tissue dissection, preserve fracture biology, and allow earlier weight-bearing. These advantages typically result in faster healing times, reduced infection rates, and better functional outcomes compared to plate fixation for appropriate fracture types.
Are there situations where intramedullary nails should not be used?
Contraindications include metaphyseal fractures involving joint surfaces, active infections at the fracture site, severe osteoporosis preventing adequate fixation, and anatomical abnormalities that preclude safe nail insertion. Open fractures with significant contamination may require alternative treatment approaches or staged procedures before intramedullary stabilization can be safely performed.