Orthopedic surgery has witnessed remarkable advances in fixation technology, with cannulated screws emerging as a sophisticated alternative to traditional solid screws. These hollow-core implants have revolutionized surgical procedures by offering enhanced precision and improved patient outcomes. The fundamental difference lies in their structural design, where cannulated screws feature a central hollow channel that allows for guided insertion over a wire, while traditional screws rely on direct placement techniques. This technological evolution has addressed many limitations associated with conventional fixation methods, particularly in complex anatomical regions where accuracy is paramount. Understanding the comparative advantages and applications of these two screw types is essential for orthopedic surgeons seeking optimal surgical outcomes.
Structural Design and Engineering Differences
Core Architecture Variations
The primary distinction between cannulated and traditional screws lies in their internal architecture. Traditional screws feature a solid core construction that provides maximum material strength throughout the entire implant length. This design offers exceptional resistance to bending and torsional forces, making them suitable for high-load applications. The solid structure distributes stress evenly across the screw body, reducing the risk of mechanical failure under extreme conditions. However, this design limits surgical flexibility and requires precise preoperative planning to ensure accurate placement.
Cannulated screws incorporate a hollow central channel that fundamentally alters their mechanical properties and surgical utility. This channel typically ranges from 1.5mm to 3.2mm in diameter, depending on the screw size and intended application. The hollow design reduces the overall material volume, which can impact load-bearing capacity compared to solid screws of equivalent external dimensions. However, this trade-off is often justified by the enhanced surgical control and precision that the guidewire system provides. The internal channel must be precisely engineered to maintain structural integrity while accommodating standard guidewires used in orthopedic procedures.
Material Composition and Manufacturing
Both screw types utilize similar biocompatible materials, primarily titanium alloys and stainless steel grades specifically designed for orthopedic applications. Titanium alloys, such as Ti-6Al-4V, offer superior biocompatibility and corrosion resistance, making them ideal for permanent implantation. The manufacturing process for traditional screws involves conventional machining or cold-forming techniques that create a uniform solid structure. Quality control measures focus on thread accuracy, surface finish, and dimensional tolerances to ensure consistent performance across production batches.
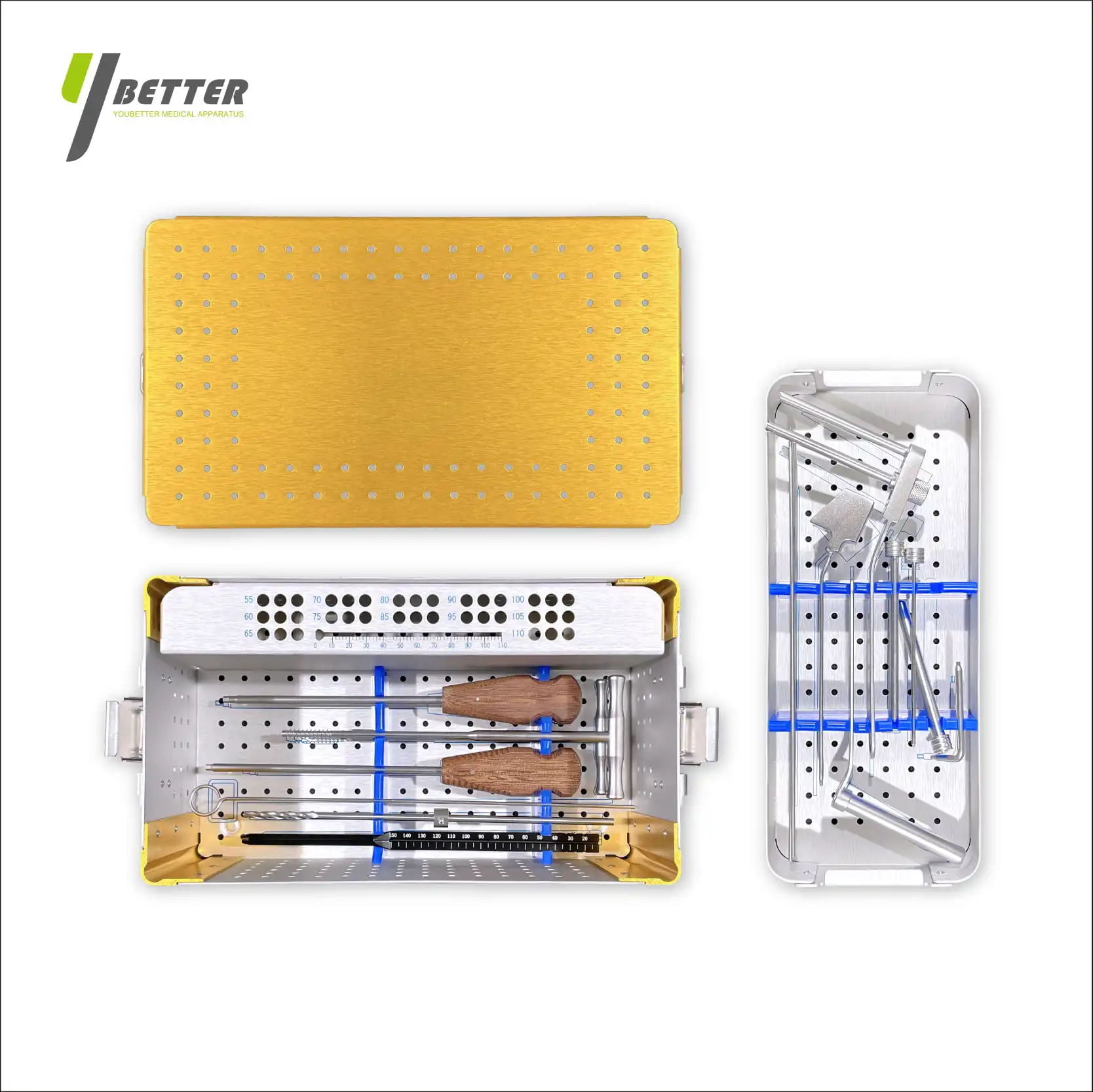
Manufacturing cannulated screws requires additional complexity due to the precise drilling and finishing of the internal channel. Advanced CNC machining techniques create the hollow core while maintaining the structural integrity of the surrounding material. The internal surface must be smooth and uniform to prevent guidewire binding or damage during insertion. Special attention is given to the screw tip design, where the cannulation must remain patent while providing effective bone penetration characteristics. Post-manufacturing inspection includes internal channel verification and guidewire compatibility testing to ensure surgical functionality.
Surgical Applications and Clinical Advantages
Precision Placement Benefits
The guidewire system used with cannulated screws provides unprecedented surgical accuracy, particularly in complex anatomical regions where traditional screw placement would be challenging. Surgeons can first establish the optimal trajectory using a thin guidewire, often under fluoroscopic guidance, before committing to final screw placement. This approach significantly reduces the risk of neurovascular injury and improves implant positioning accuracy. The ability to verify trajectory and depth before final insertion is especially valuable in procedures involving the spine, pelvis, and other critical anatomical structures.
Traditional screws require direct placement based on anatomical landmarks and imaging guidance, which can be less precise in certain clinical scenarios. While experienced surgeons achieve excellent results with traditional techniques, the margin for error is often smaller, particularly in revision surgeries or cases with distorted anatomy. The immediate tactile feedback from traditional screw insertion can provide valuable information about bone quality and engagement, but this advantage must be weighed against the potential for placement errors in challenging anatomical locations.
Minimally Invasive Surgery Compatibility
Cannulated screws excel in minimally invasive surgical approaches where direct visualization is limited. The guidewire technique allows for accurate screw placement through small incisions, reducing soft tissue trauma and promoting faster recovery times. This capability has made cannulated screws particularly popular in procedures such as percutaneous fixation of fractures and minimally invasive spinal fusion techniques. The reduced surgical exposure minimizes blood loss, decreases infection risk, and often results in shorter hospital stays for patients.
While traditional screws can be used in minimally invasive procedures, they often require more extensive surgical exposure to ensure accurate placement. The inability to pre-verify trajectory with a guidewire can necessitate larger incisions to provide adequate visualization and instrument access. However, traditional screws may offer advantages in cases where maximum mechanical strength is required, and the surgical approach allows for direct visualization and manual palpation of anatomical structures.

Mechanical Performance and Load Distribution
Strength Characteristics Comparison
The mechanical properties of cannulated versus traditional screws present important considerations for clinical decision-making. Traditional screws generally demonstrate superior ultimate tensile strength and fatigue resistance due to their solid cross-sectional area. The continuous material distribution provides optimal load transfer and resistance to cyclic loading conditions commonly encountered in orthopedic applications. Biomechanical testing consistently shows that solid screws can withstand higher peak loads before failure, making them preferable in high-stress applications such as major load-bearing joints or spine instrumentation where maximum strength is paramount.
Cannulated screws exhibit reduced cross-sectional area due to their hollow core, which directly impacts their load-bearing capacity. The magnitude of strength reduction varies depending on the cannulation diameter relative to the outer screw diameter, typically ranging from 15-30% reduction in ultimate strength compared to solid screws of equivalent size. However, this reduction may be clinically acceptable in many applications where the enhanced surgical precision outweighs the mechanical trade-offs. Modern cannulated screw designs incorporate engineering optimizations to minimize strength reduction while maintaining functional cannulation diameter.
Stress Distribution Patterns
The hollow core of cannulated screws creates altered stress distribution patterns under loading conditions. Finite element analysis studies reveal that stress concentrations occur at the inner surface of the cannulation, particularly near thread roots where material thickness is minimal. These stress risers can potentially initiate crack propagation under cyclic loading, although clinical failure rates remain low when screws are used within their designed parameters. The stress distribution also varies along the screw length, with the greatest concentrations typically occurring at the thread-bone interface where load transfer is most critical.
Traditional screws demonstrate more uniform stress distribution throughout their solid cross-section, with peak stresses occurring at the thread-bone interface as expected. The absence of internal discontinuities reduces the likelihood of stress concentration-induced failures. However, the clinical significance of these mechanical differences depends heavily on the specific application, loading conditions, and patient factors. Many cannulated screw applications involve relatively low-stress environments where the mechanical advantages of solid screws may not be clinically relevant.
Cost Analysis and Economic Considerations
Manufacturing and Production Costs
The production of cannulated screws involves additional manufacturing complexity that directly impacts their cost structure. The precision drilling and finishing of the internal channel requires specialized tooling and extended machining time compared to traditional solid screws. Quality control procedures are more extensive, including internal channel inspection and guidewire compatibility verification. These manufacturing requirements typically result in 20-40% higher production costs for cannulated screws, depending on the specific design and quality standards. However, volume production and manufacturing efficiency improvements have helped reduce this cost differential over time.
Traditional screws benefit from simpler manufacturing processes and established production workflows that have been optimized over decades of use. The absence of internal features allows for more efficient machining or forming operations, resulting in lower per-unit production costs. Economies of scale are more easily achieved with traditional screw production due to the standardized manufacturing requirements. However, the cost advantage of traditional screws must be evaluated against the potential benefits of improved surgical outcomes and reduced complications that cannulated screws may provide in appropriate applications.
Healthcare System Impact
The economic evaluation of cannulated versus traditional screws extends beyond initial implant costs to include surgical efficiency and patient outcome considerations. Cannulated screws may reduce operative time in certain procedures due to improved placement accuracy and reduced need for repositioning. The enhanced precision can potentially decrease complication rates, leading to reduced revision surgery requirements and associated healthcare costs. Shorter operative times also translate to reduced operating room utilization costs and improved surgical suite efficiency.
Hospital procurement decisions increasingly consider total cost of ownership rather than simply initial implant pricing. The improved surgical outcomes and potential for reduced complications with cannulated screws may justify their higher acquisition cost through reduced overall episode costs. However, this economic analysis must be procedure-specific and institution-specific, as the benefits may not be uniformly applicable across all orthopedic applications. Cost-effectiveness studies continue to evaluate the long-term economic impact of these different fixation technologies.
Clinical Outcomes and Patient Benefits
Surgical Success Rates
Clinical studies comparing cannulated and traditional screws have shown procedure-specific variations in outcomes, with neither option demonstrating universal superiority across all applications. In procedures requiring high precision, such as scaphoid fracture fixation or femoral neck fracture repair, cannulated screws have shown improved placement accuracy and reduced complication rates. The ability to verify trajectory before final placement has contributed to lower rates of neurovascular injury and improved fracture reduction quality. Long-term follow-up studies indicate comparable healing rates between the two screw types when appropriately selected for specific clinical scenarios.
Traditional screws continue to demonstrate excellent clinical outcomes in applications where their superior mechanical strength is advantageous. Major load-bearing applications, such as large joint reconstructions or spinal instrumentation, often favor traditional screws due to their enhanced fatigue resistance and ultimate strength characteristics. The clinical experience with traditional screws spans several decades, providing extensive outcome data and refined surgical techniques. Surgeon familiarity and training with traditional screw placement techniques may also influence clinical outcomes in some cases.
Patient Recovery and Quality of Life
The minimally invasive capabilities of cannulated screws often translate to improved patient recovery experiences. Reduced surgical trauma, smaller incisions, and shorter operative times contribute to decreased postoperative pain and faster return to normal activities. Patient satisfaction scores frequently reflect these benefits, particularly in procedures where cosmetic concerns are important. The reduced soft tissue disruption associated with guidewire-assisted placement can lead to preserved muscle function and reduced scarring compared to traditional open approaches sometimes required for accurate solid screw placement.
Recovery timelines may favor cannulated screw procedures in appropriate cases, though the specific benefits depend on the surgical indication and patient factors. Reduced surgical morbidity can translate to shorter hospital stays, earlier mobilization, and faster return to work or recreational activities. However, the long-term functional outcomes are generally comparable between properly placed cannulated and traditional screws, with implant selection being more influential than screw type in determining final patient satisfaction and functional recovery.
FAQ
What are the main advantages of cannulated screws over traditional screws?
Cannulated screws offer several key advantages including enhanced surgical precision through guidewire-assisted placement, improved accuracy in complex anatomical regions, compatibility with minimally invasive surgical techniques, and reduced risk of neurovascular injury. The hollow design allows surgeons to verify trajectory and positioning before final screw insertion, which is particularly valuable in challenging cases or revision surgeries. These benefits often outweigh the slight reduction in mechanical strength compared to solid screws.
Are cannulated screws weaker than traditional solid screws?
Cannulated screws do have reduced cross-sectional area due to their hollow core, resulting in approximately 15-30% lower ultimate tensile strength compared to solid screws of equivalent outer diameter. However, this strength reduction is often clinically acceptable for many orthopedic applications. The decision should be based on the specific loading requirements of the procedure, with solid screws preferred for high-stress applications and cannulated screws chosen when surgical precision is paramount.
When should surgeons choose traditional screws over cannulated screws?
Traditional screws are preferred in high-load bearing applications where maximum mechanical strength is essential, such as major joint reconstructions, heavy-duty spinal instrumentation, or cases involving poor bone quality where enhanced pullout strength is crucial. They are also appropriate when direct surgical visualization is adequate for accurate placement and when cost considerations are a primary factor. The solid design provides optimal fatigue resistance for long-term implantation in demanding mechanical environments.
How do the costs compare between cannulated and traditional screws?
Cannulated screws typically cost 20-40% more than traditional screws due to their more complex manufacturing requirements and additional quality control procedures. However, the total cost analysis should include potential benefits such as reduced operative time, lower complication rates, and improved surgical outcomes. Many healthcare systems find that the enhanced precision and reduced revision surgery requirements of cannulated screws can justify their higher initial cost through improved overall episode economics and patient satisfaction.