Orthopedic surgery has undergone remarkable transformation with the introduction of advanced trauma implants, revolutionizing how surgeons approach complex fracture repairs and bone reconstruction procedures. These sophisticated medical devices have become indispensable tools in modern orthopedic practice, offering unprecedented precision and reliability in treating traumatic injuries. The evolution of trauma implants represents a significant leap forward in surgical technology, enabling healthcare professionals to achieve superior patient outcomes while reducing recovery times and complications. Understanding the multifaceted benefits of these innovative solutions is crucial for both medical professionals and patients seeking optimal treatment options for orthopedic conditions.
Advanced Materials and Design Innovation
Titanium Alloy Engineering
Modern trauma implants utilize cutting-edge titanium alloys that offer exceptional biocompatibility and mechanical strength, ensuring long-term stability within the human body. These materials demonstrate superior corrosion resistance and osseointegration properties, allowing bone tissue to naturally bond with the implant surface over time. The lightweight nature of titanium alloys reduces stress on surrounding tissues while maintaining the structural integrity required for supporting significant mechanical loads during patient recovery and daily activities.
Manufacturing processes for titanium-based trauma implants have evolved to incorporate precise surface treatments that promote cellular adhesion and accelerate healing responses. Advanced surface texturing techniques create optimal environments for bone cell proliferation, significantly improving the integration process between implant and natural bone tissue. This enhanced biocompatibility translates directly into reduced rejection rates and improved long-term surgical outcomes for patients.
Anatomical Precision Engineering
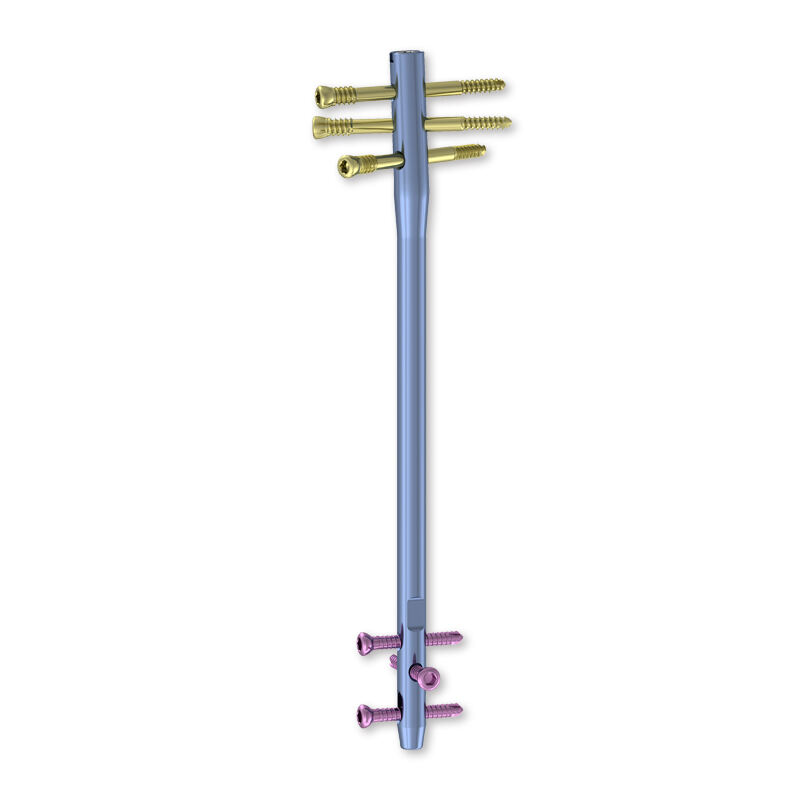
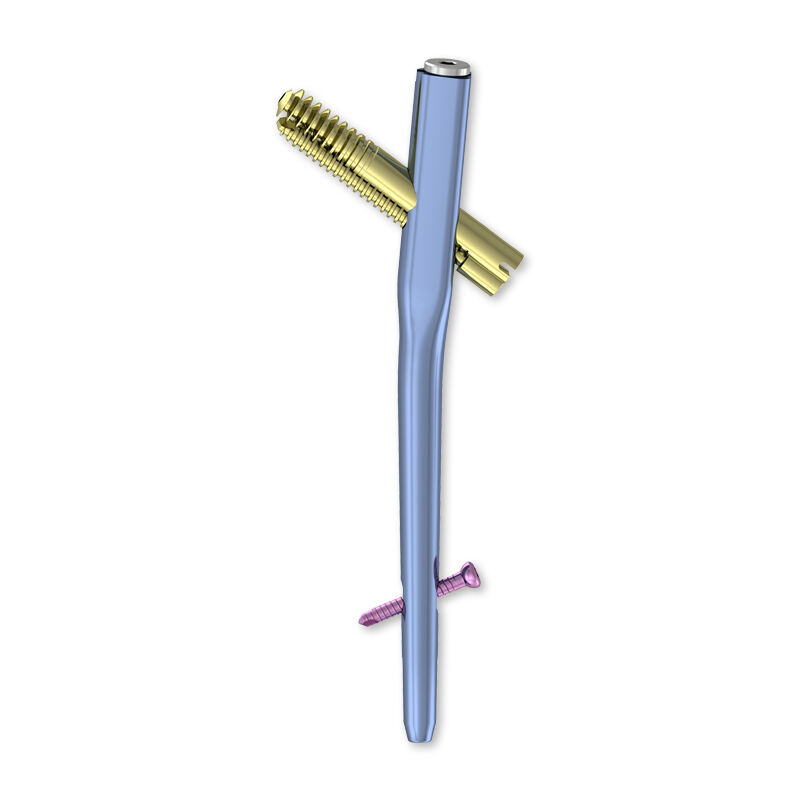
Contemporary trauma implants are designed with anatomical precision, utilizing three-dimensional modeling and computer-aided design technologies to create patient-specific solutions. These implants conform closely to natural bone geometry, reducing surgical complexity and improving the accuracy of implant placement during procedures. The precision engineering ensures optimal load distribution across the fracture site, promoting faster healing and reducing the risk of implant failure.
Customization capabilities allow surgeons to select implants that match individual patient anatomy, accommodating variations in bone size, shape, and density characteristics. This personalized approach enhances surgical outcomes by ensuring proper fit and function, ultimately leading to improved patient satisfaction and reduced revision surgery requirements. The anatomical design philosophy represents a significant advancement over traditional generic implant solutions.
Surgical Technique Enhancement
Minimally Invasive Procedures
The development of specialized trauma implants has enabled surgeons to adopt minimally invasive surgical techniques, significantly reducing tissue damage and accelerating patient recovery timelines. These procedures require smaller incisions and less soft tissue dissection, resulting in reduced post-operative pain and improved cosmetic outcomes. The precision design of modern implants facilitates accurate placement through smaller surgical approaches, maintaining therapeutic effectiveness while minimizing surgical trauma.
Advanced instrumentation systems work in conjunction with trauma implants to provide surgeons with enhanced control and precision during procedures. Specialized delivery systems and positioning guides ensure accurate implant placement, reducing operative time and improving consistency across different surgical cases. This technological integration has transformed complex fracture repairs into more predictable and successful procedures.
Real-Time Imaging Integration
Modern trauma implants are designed to be compatible with advanced imaging technologies, allowing surgeons to monitor implant placement and healing progress with unprecedented clarity. Intraoperative imaging systems provide real-time feedback during surgery, enabling immediate adjustments and ensuring optimal implant positioning. This integration reduces the likelihood of revision surgeries and improves overall treatment outcomes.
Post-operative imaging compatibility ensures that healthcare providers can effectively monitor healing progress and identify potential complications early in the recovery process. The radiopaque properties of trauma implants allow for clear visualization on standard radiographic equipment, facilitating routine follow-up assessments and long-term patient monitoring protocols.
Clinical Outcomes and Recovery Benefits
Accelerated Bone Healing
Clinical studies consistently demonstrate that modern trauma implants significantly accelerate bone healing processes compared to traditional treatment methods. The optimized mechanical properties of these devices provide appropriate stability while allowing controlled micro-motion that stimulates natural bone formation. This balanced approach promotes faster callus formation and more robust bone union at fracture sites.
Bioactive coatings on trauma implants further enhance healing by releasing growth factors and promoting cellular activities essential for bone regeneration. These advanced surface treatments create favorable environments for osteoblast activity, leading to improved bone quality and faster integration between implant and natural tissue. The result is reduced healing times and stronger, more durable bone repair outcomes.
Reduced Complication Rates
The implementation of advanced trauma implants has led to measurable reductions in post-surgical complications, including infection rates, implant loosening, and mechanical failures. Improved design features such as optimized screw trajectories and enhanced fixation mechanisms provide superior stability throughout the healing process. These enhancements translate into fewer revision surgeries and improved long-term patient outcomes.
Antimicrobial surface treatments incorporated into many trauma implants help prevent bacterial colonization and reduce the risk of post-operative infections. These protective coatings maintain their effectiveness throughout the critical healing period, providing an additional layer of protection against complications that could compromise surgical success. The combination of superior design and antimicrobial properties represents a comprehensive approach to complication prevention.
Patient Quality of Life Improvements
Enhanced Functional Recovery
Patients receiving modern trauma implants experience significantly improved functional recovery outcomes, with faster return to normal activities and reduced long-term disability rates. The superior mechanical properties and anatomical design of these devices restore natural joint biomechanics more effectively than traditional treatment approaches. This restoration of normal function is particularly important for active individuals seeking to return to demanding physical activities.
Range of motion preservation is enhanced through the use of trauma implants that maintain proper joint alignment and stability during healing. The precise fit and superior fixation provided by these devices prevent malunion and other complications that could limit long-term joint function. Patients report higher satisfaction levels and improved quality of life outcomes when treated with advanced trauma implant systems.
Long-Term Durability
The exceptional durability of contemporary trauma implants ensures long-lasting therapeutic benefits for patients, with many devices designed to provide lifetime functionality. Advanced materials and manufacturing processes create implants capable of withstanding millions of loading cycles without mechanical failure or degradation. This durability reduces the need for revision surgeries and provides patients with confidence in their long-term treatment outcomes.
Fatigue resistance testing demonstrates that modern trauma implants maintain their mechanical properties over extended periods, even under demanding physiological loading conditions. The combination of superior materials and optimized design features ensures that implants continue to provide stable fixation and support throughout the patient's lifetime, representing excellent value for healthcare investments.
Economic Impact and Healthcare Efficiency
Cost-Effectiveness Analysis
While trauma implants represent a significant initial investment, comprehensive cost-effectiveness analyses demonstrate substantial long-term economic benefits for healthcare systems. The reduced complication rates and faster recovery times associated with these devices translate into lower overall treatment costs and improved resource utilization. Healthcare facilities report decreased length of stay and reduced readmission rates for patients treated with advanced trauma implant systems.
The prevention of revision surgeries through the use of superior trauma implants generates significant cost savings over time, eliminating the need for additional procedures and extended rehabilitation periods. These economic benefits extend beyond direct medical costs to include reduced productivity losses and improved patient quality of life metrics. Healthcare policymakers increasingly recognize trauma implants as cost-effective solutions for managing complex orthopedic injuries.
Workflow Optimization
Advanced trauma implants contribute to improved surgical workflow efficiency through standardized instrumentation systems and simplified surgical techniques. Operating room time is reduced due to the precision and reliability of modern implant systems, allowing facilities to increase surgical volume while maintaining high quality outcomes. This efficiency improvement benefits both healthcare providers and patients seeking timely treatment for traumatic injuries.
Training requirements for surgical teams are streamlined through the use of intuitive trauma implant systems that incorporate user-friendly design features and comprehensive educational resources. Reduced learning curves for new procedures enable healthcare facilities to adopt advanced techniques more rapidly and ensure consistent outcomes across different surgical teams. This standardization improves overall care quality and reduces variability in treatment results.
Future Developments and Innovations
Smart Implant Technology
Emerging smart trauma implants incorporate sensors and monitoring capabilities that provide real-time feedback on healing progress and implant performance. These devices can detect changes in loading patterns, temperature variations, and other physiological parameters that indicate healing status or potential complications. The integration of wireless communication technologies allows for remote monitoring and early intervention when necessary.
Artificial intelligence algorithms are being developed to analyze data from smart trauma implants, providing predictive insights that can guide treatment decisions and optimize patient outcomes. These advanced systems will enable personalized treatment protocols based on individual healing patterns and risk factors, representing the next evolution in orthopedic care delivery.
Biodegradable Materials
Research into biodegradable trauma implants focuses on developing materials that provide temporary support during healing before being naturally absorbed by the body. These innovative solutions eliminate the need for implant removal procedures while maintaining the mechanical properties required for effective fracture fixation. Biodegradable implants represent a paradigm shift toward more natural healing processes and reduced long-term implant burden.
Controlled degradation rates can be engineered to match specific healing timelines, ensuring that implant support is maintained throughout the critical healing period before gradual absorption begins. This approach reduces foreign body presence while providing optimal therapeutic benefits, appealing to patients seeking more natural treatment alternatives.
FAQ
What are the main advantages of trauma implants over traditional fracture treatment methods
Trauma implants offer superior stability and precision compared to traditional casting or external fixation methods, leading to faster healing times and better functional outcomes. These devices provide internal support directly at the fracture site, allowing for earlier mobilization and reduced risk of complications such as malunion or nonunion. The biocompatible materials used in modern trauma implants integrate naturally with bone tissue, creating strong, durable repairs that restore normal anatomical function.
How long do trauma implants typically last in the body
Modern trauma implants are designed for lifetime use, with advanced materials and manufacturing processes ensuring durability over decades of normal physiological loading. Clinical studies show that high-quality trauma implants can function effectively for 20-30 years or more without requiring replacement. The longevity depends on factors such as patient activity level, bone quality, and adherence to post-operative care protocols, but most patients can expect their trauma implants to provide permanent fixation.
Are there any risks or complications associated with trauma implants
While trauma implants have excellent safety profiles, potential risks include infection, implant loosening, and rare allergic reactions to implant materials. Modern implants incorporate antimicrobial coatings and improved design features that significantly reduce these risks compared to older generation devices. Proper surgical technique and post-operative care further minimize complication rates, with most patients experiencing successful outcomes without significant adverse events.
What is the recovery process like after trauma implant surgery
Recovery from trauma implant surgery typically involves a structured rehabilitation program that begins with protected weight-bearing and gradually progresses to full activity levels. Most patients can begin gentle movement within days of surgery, with complete healing occurring over 3-6 months depending on the specific injury and implant type. Physical therapy plays a crucial role in optimizing recovery outcomes, helping patients regain strength, mobility, and function while ensuring proper healing around the trauma implants.