Modern medical technology has revolutionized the field of orthopedic surgery, particularly in the development and application of trauma implants. These sophisticated medical devices have become essential tools for surgeons treating complex fractures, bone defects, and skeletal injuries. The evolution of trauma implants represents one of the most significant advances in contemporary medicine, offering patients improved outcomes and faster recovery times. Understanding the materials used in these implants and their specific advantages is crucial for healthcare professionals, patients, and industry stakeholders who seek to make informed decisions about treatment options.
The selection of appropriate materials for trauma implants involves careful consideration of biocompatibility, mechanical properties, corrosion resistance, and long-term durability. Medical device manufacturers and orthopedic surgeons must evaluate multiple factors when choosing materials for specific applications, ensuring that each implant meets the demanding requirements of human physiology. The continuous advancement in material science has led to the development of increasingly sophisticated trauma implants that offer superior performance and patient outcomes.
Titanium and Its Alloys in Trauma Applications
Pure Titanium Properties and Benefits
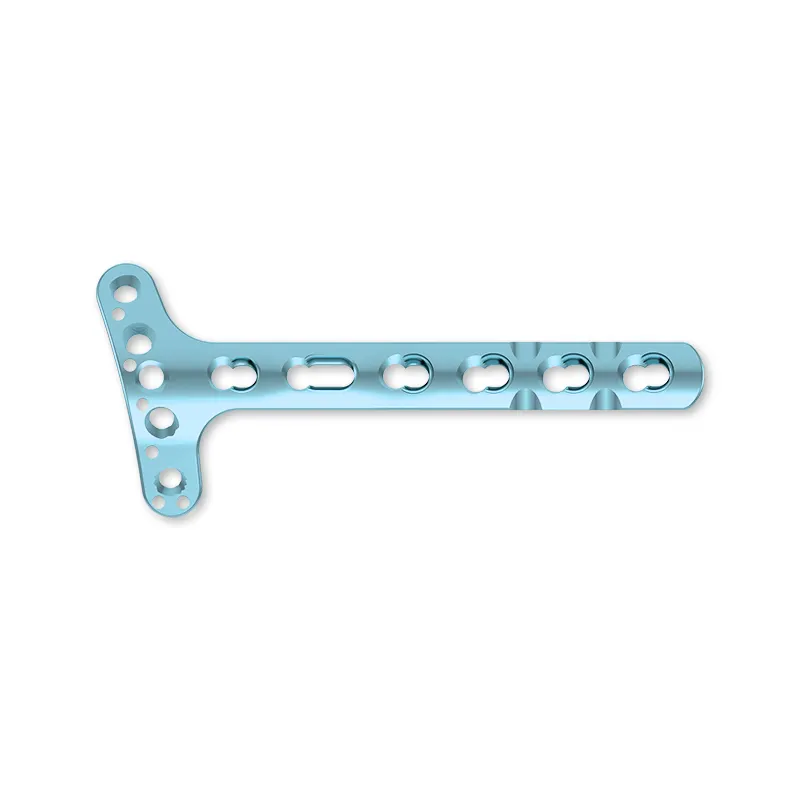
Pure titanium stands as one of the most widely used materials in modern trauma implants due to its exceptional biocompatibility and corrosion resistance. This metal exhibits remarkable compatibility with human tissue, rarely causing adverse reactions or rejection responses in patients. The low elastic modulus of titanium closely matches that of human bone, reducing stress shielding effects that can lead to bone resorption around implant sites. Medical professionals particularly value titanium's ability to osseointegrate, allowing bone tissue to grow directly onto the implant surface and creating a strong, permanent bond.
The corrosion resistance of pure titanium stems from its natural oxide layer, which forms spontaneously when exposed to oxygen. This protective barrier prevents the release of metallic ions into surrounding tissues, minimizing the risk of inflammatory responses and long-term complications. Additionally, titanium's radiolucency properties enable clear visualization during post-operative imaging procedures, allowing surgeons to monitor healing progress and detect potential complications more effectively.
Titanium Alloy Compositions and Applications
Titanium alloys, particularly Ti-6Al-4V, represent a significant advancement in trauma implant technology, offering enhanced mechanical properties while maintaining excellent biocompatibility. This alloy composition combines titanium with aluminum and vanadium to create a material with superior strength-to-weight ratio and fatigue resistance. The addition of these alloying elements increases the material's yield strength and ultimate tensile strength, making it ideal for load-bearing applications such as femoral nails, bone plates, and spinal rods.
Recent developments in titanium alloy technology have led to the creation of beta-titanium alloys, which offer even lower elastic modulus values closer to human bone. These advanced alloys provide improved biomechanical compatibility and reduced stress shielding effects, particularly beneficial in long-term implant applications. The versatility of titanium alloys allows manufacturers to tailor material properties for specific anatomical locations and patient requirements, ensuring optimal performance across diverse trauma scenarios.
Stainless Steel Applications in Orthopedic Surgery
316L Stainless Steel Characteristics
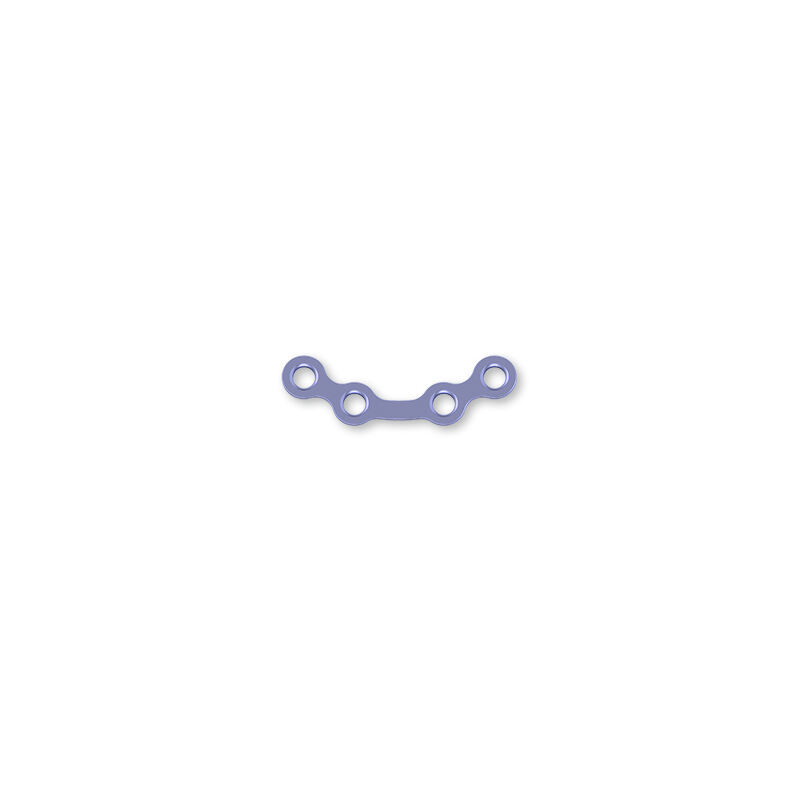
316L stainless steel remains a cornerstone material in trauma implant manufacturing, particularly for temporary fixation devices and cost-effective solutions. This austenitic stainless steel variant offers excellent mechanical properties, including high tensile strength and good ductility, making it suitable for various orthopedic applications. The low carbon content in 316L stainless steel enhances its corrosion resistance and reduces the risk of carbide precipitation, which could compromise the material's integrity over time.
The magnetic properties of 316L stainless steel, while generally considered MRI-compatible, require careful consideration in patients who may require frequent magnetic resonance imaging. Despite this limitation, the material's proven track record, cost-effectiveness, and reliable performance continue to make it a popular choice for certain trauma implants, particularly in healthcare systems with budget constraints or for applications where titanium may be unnecessary.
Surface Treatments and Coating Technologies
Advanced surface treatment techniques have significantly improved the performance of stainless steel trauma implants, addressing some of the material's inherent limitations. Electropolishing processes create smooth, uniform surfaces that reduce bacterial adhesion and improve corrosion resistance. These treatments also eliminate surface irregularities that could serve as stress concentration points, potentially leading to implant failure under cyclic loading conditions.
Coating technologies, including diamond-like carbon coatings and titanium nitride layers, further enhance the biocompatibility and wear resistance of stainless steel implants. These surface modifications can significantly reduce ion release rates and improve the long-term stability of the implant-tissue interface. The development of bioactive coatings also enables stainless steel implants to promote bone growth and integration, expanding their applications in trauma surgery.
Cobalt-Chromium Alloys for High-Performance Applications
Mechanical Properties and Durability
Cobalt-chromium alloys represent the pinnacle of mechanical performance in trauma implant materials, offering exceptional strength, wear resistance, and fatigue life. These alloys demonstrate superior resistance to crack propagation and can withstand extreme loading conditions encountered in high-stress anatomical locations. The excellent wear characteristics of cobalt-chromium make it particularly suitable for articulating surfaces and components that experience repetitive motion or high contact stresses.
The exceptional corrosion resistance of cobalt-chromium alloys results from the formation of a stable chromium oxide layer on the surface. This protective layer remains intact even under challenging physiological conditions, preventing the release of metallic ions and maintaining implant integrity over extended periods. The combination of mechanical strength and corrosion resistance makes cobalt-chromium alloys ideal for demanding trauma applications where implant longevity is critical.
Biocompatibility Considerations and Clinical Applications
While cobalt-chromium alloys offer outstanding mechanical properties, their biocompatibility profile requires careful evaluation, particularly in patients with known metal sensitivities. The potential for cobalt and chromium ion release has led to increased scrutiny of these materials in certain applications. However, when properly designed and manufactured, cobalt-chromium trauma implants demonstrate excellent long-term biocompatibility and clinical performance.
The use of cobalt-chromium alloys in trauma applications typically focuses on high-load bearing components such as femoral stems, acetabular shells, and complex reconstructive devices. The material's ability to maintain dimensional stability under extreme conditions makes it invaluable for cases involving severe trauma or revision procedures where maximum mechanical performance is essential for successful outcomes.
Emerging Materials and Advanced Technologies
Biodegradable Polymer Systems
Biodegradable polymers represent a revolutionary approach to trauma implant design, offering the unique advantage of gradual resorption as healing progresses. These materials eliminate the need for secondary removal surgeries and reduce long-term complications associated with permanent implants. Poly-L-lactic acid, polyglycolic acid, and their copolymers demonstrate excellent biocompatibility and controllable degradation rates, allowing surgeons to match implant resorption with bone healing timelines.
The development of reinforced biodegradable composites has expanded the applications of these materials in trauma surgery. By incorporating ceramic particles or continuous fibers, manufacturers can enhance the mechanical properties of biodegradable polymers while maintaining their resorbable characteristics. These advanced materials show particular promise in pediatric applications, where growing bone structures benefit from temporary support that gradually transfers load back to natural tissue.
Additive Manufacturing and Customization
Three-dimensional printing technologies have revolutionized the production of trauma implants, enabling unprecedented levels of customization and geometric complexity. Additive manufacturing allows for the creation of patient-specific implants tailored to individual anatomical variations, improving fit and reducing surgical complications. The ability to incorporate porous structures and complex internal geometries enhances osseointegration and reduces implant weight while maintaining mechanical integrity.
The integration of additive manufacturing with advanced materials science has led to the development of functionally graded implants that vary in properties across their structure. These sophisticated devices can provide optimal mechanical properties at stress concentration points while maintaining flexibility in areas requiring natural bone movement. The rapid prototyping capabilities of 3D printing also accelerate the development and testing of new trauma implant designs, reducing time to market for innovative solutions.
Material Selection Criteria and Clinical Considerations
Biomechanical Compatibility Factors
The selection of appropriate materials for trauma implants requires comprehensive evaluation of biomechanical compatibility factors that directly influence clinical outcomes. Elastic modulus matching between implant materials and human bone tissue plays a crucial role in preventing stress shielding and promoting healthy bone remodeling. Materials with elastic moduli significantly higher than bone can lead to bone resorption and implant loosening over time, while excessively flexible materials may provide inadequate support during healing.
Fatigue resistance represents another critical consideration, as trauma implants must withstand millions of loading cycles throughout their service life. The ability of materials to resist crack initiation and propagation under repetitive loading determines the long-term reliability of implant systems. Advanced testing protocols and finite element analysis help predict material behavior under physiological loading conditions, enabling informed material selection decisions.
Patient-Specific Material Considerations
Individual patient factors significantly influence material selection for trauma implants, requiring personalized approaches to optimize outcomes. Age-related considerations include bone quality, healing capacity, and expected implant longevity requirements. Younger patients may benefit from biodegradable materials that allow for natural bone remodeling, while older patients might require more durable permanent solutions with proven long-term performance records.
Activity level and lifestyle factors also guide material selection decisions, as highly active patients place greater demands on implant systems. Professional athletes or manual laborers may require materials with superior fatigue resistance and wear properties, while sedentary patients might achieve excellent outcomes with less robust but more cost-effective material options. Allergy histories and sensitivity testing help identify patients who may require alternative materials to prevent adverse reactions.
Quality Control and Regulatory Standards
Manufacturing Standards and Certification
Rigorous quality control measures ensure that trauma implant materials meet the exacting standards required for medical applications. International standards such as ISO 13485 and FDA regulations establish comprehensive frameworks for material testing, manufacturing processes, and quality assurance procedures. These standards mandate extensive biocompatibility testing, mechanical property verification, and sterility validation to ensure patient safety and implant reliability.
Material traceability systems track every aspect of the manufacturing process, from raw material sourcing through final product distribution. This comprehensive documentation enables rapid identification and resolution of any quality issues that may arise, protecting patient safety and maintaining confidence in trauma implant systems. Advanced testing protocols, including surface analysis, mechanical testing, and biological evaluation, provide multiple layers of quality assurance.
Post-Market Surveillance and Performance Monitoring
Ongoing monitoring of trauma implant performance provides valuable feedback for material selection and design optimization. Post-market surveillance systems collect data on clinical outcomes, revision rates, and material-related complications to identify trends and potential issues. This information helps manufacturers refine material properties and processing techniques while providing surgeons with evidence-based guidance for material selection.
Long-term studies tracking implant performance over decades provide insights into material behavior and patient outcomes that inform future material development efforts. Registry data from various international databases enable comparison of different materials and designs, supporting evidence-based decision making in trauma surgery. The continuous feedback loop between clinical experience and material development drives ongoing improvements in trauma implant technology.
FAQ
What are the main advantages of titanium over other materials in trauma implants
Titanium offers superior biocompatibility with minimal risk of allergic reactions, excellent corrosion resistance due to its natural oxide layer, and an elastic modulus closer to bone tissue that reduces stress shielding effects. Additionally, titanium's radiolucency allows for better post-operative imaging, and its osseointegration properties promote strong bone-implant bonding for long-term stability.
How do biodegradable materials compare to permanent implants in trauma applications
Biodegradable materials eliminate the need for implant removal surgeries and reduce long-term complications associated with permanent foreign bodies. They gradually transfer load back to healing bone tissue and are particularly beneficial in pediatric applications. However, they currently have limited mechanical strength compared to metal implants and are primarily suitable for specific applications where temporary support is sufficient.
What factors determine the choice between stainless steel and titanium for trauma implants
The choice depends on several factors including cost considerations, expected implant duration, patient age and activity level, and anatomical location. Stainless steel offers cost-effectiveness for temporary applications but has higher elastic modulus and potential MRI compatibility issues. Titanium provides superior biocompatibility and long-term performance but at higher cost, making it preferred for permanent implants and younger patients.
How do surface treatments improve the performance of trauma implant materials
Surface treatments enhance implant performance by improving corrosion resistance, reducing bacterial adhesion, promoting osseointegration, and minimizing wear. Techniques such as electropolishing create smooth surfaces that reduce stress concentrations, while bioactive coatings can stimulate bone growth. These treatments allow optimization of surface properties while maintaining the bulk material's mechanical characteristics.
Table of Contents
- Titanium and Its Alloys in Trauma Applications
- Stainless Steel Applications in Orthopedic Surgery
- Cobalt-Chromium Alloys for High-Performance Applications
- Emerging Materials and Advanced Technologies
- Material Selection Criteria and Clinical Considerations
- Quality Control and Regulatory Standards
-
FAQ
- What are the main advantages of titanium over other materials in trauma implants
- How do biodegradable materials compare to permanent implants in trauma applications
- What factors determine the choice between stainless steel and titanium for trauma implants
- How do surface treatments improve the performance of trauma implant materials